In many jurisdictions around the world, drug laws are changing in favor of legalizing medical and non-medical personal use of marijuana. Although it is premature to say with certainty if or how these changes are affecting the public’s health, researchers continue to examine marijuana use for potential harmful consequences. Such examinations are essential to the successful treatment of Cannabis Use Disorder. This week, STASH reviews recent research related to marijuana withdrawal’s impact on adolescent treatment seekers (Greene & Kelly, in press).
Method
- Participants included 127 adolescent outpatient substance use disorder (SUD) treatment seekers (71% of those who presented for treatment).
- The analytic sample consisted of 90 participants who reported cannabis to be their drug of choice.
- Participants completed baseline and 3-, 6-, and 12-month surveys that assessed factors such as, demographics, substance use problem recognition, withdrawal experiences (i.e., reporting at least one symptom of withdrawal or using drugs to relieve withdrawal), substance use severity, and more.
- Participant retention was 93%, 90%, and 84% at 3-, 6-, and 12-month surveys, respectively.
- Researchers (1) identified the proportion of participants who experienced cannabis withdrawal (e.g., difficulty sleeping, headaches, and feeling irritable), (2) examined baseline correlates of the experience of cannabis withdrawal, and (3) examined the relationship between cannabis withdrawal and treatment outcomes (e.g., percentage days abstinent) for one year.
Results
- About 40% of participants reported experiencing cannabis withdrawal during the past 90 days.
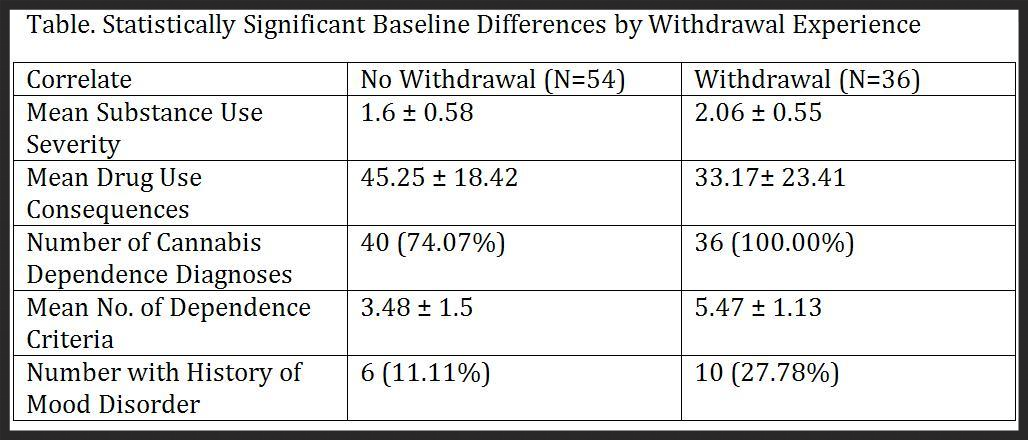
- The researchers observed some correlates of the experience of cannabis withdrawal.
- Compared to those who did not report withdrawal, those who experienced withdrawal reported higher substance use severity, more drug use consequences, and more dependence symptoms; and were more likely to meet criteria for cannabis dependence and report a history of mood disorder. See Table
- .However, experience of withdrawal was not associated with demographics, non-mood psychiatric disorder, other past 90-day substance use, other clinical characteristics (e.g., problem recognition).
- Cannabis withdrawal had a complicated relationship with treatment outcomes.
- Those who reported experiencing cannabis withdrawal at baseline reported a quicker drop in substance-use consequences and severity than those who did not.
- Over time, percent days abstinent and psychiatric symptoms were similar for those with and without cannabis withdrawal experiences.
Figure. Click image to enlarge.
Limitations
- The role of treatment completion is unclear because the authors did not report study participants’ ongoing treatment enrollment at each follow up.
- If those who reported withdrawal also have shorter treatment periods, it is not possible to determine whether the findings relate to treatment duration or withdrawal experience.
- The study relates the experiences of adolescents who are treatment seekers at a single clinical site. Non-treatment seekers and those from other sites might yield different outcomes.
Conclusions
This study shows that stopping marijuana is associated with non-trivial withdrawal experiences for a minority of users. Importantly, experiences of withdrawal might serve as markers for other problems that could impact treatment outcomes, such as having a mood disorder. As cannabis use gains acceptability among the general population, it is important to be vigilant about potential consequences of increased access in the short and long term.
– Debi LaPlante
What do you think? Please use the comment link below to provide feedback on this article.
Reference
Green, M. C. & Kelly, J. F. (in press). The prevalence of cannabis withdrawal and its influence on adolescents’ treatment response and outcomes: A 12-month prospective investigation. Journal of Addiction Medicine.