More than half of women who smoke cigarettes will quit smoking immediately before or during pregnancy. However, many end up resuming smoking in the postpartum period. Research has identified many predictors of return-to-smoking but less is known about the trajectory of smoking resumption. This week, ASHES reviews a study by Natacha M. De Genna and colleagues that investigated the distinct trajectories of return-to-smoking within 1 year postpartum among people who quit smoking during pregnancy.
What were the research questions?
What are the distinct trajectories of return-to-smoking within 1 year postpartum among people who quit smoking during pregnancy? What factors predict membership in different trajectory groups?
What did the researchers do?
The researchers conducted a secondary data analysis of 280 participants enrolled in a randomized control trial on postpartum smoking resumption prevention. The researchers recruited participants who had quit smoking during pregnancy and were motivated to remain abstinent. Postpartum smoking status was assessed at 12-, 24-, and 52-weeks via self-report and with exhaled air-samples of carbon monoxide. Participants also indicated their lifetime history of smoking, prior quit attempts, and motivations to quit. The researchers used group-based trajectory analysis to identify distinct trajectories of smoking resumption during 1 year postpartum and examined factors that predicted trajectory group membership.
What did they find?
Four distinct trajectories of return-to-smoking emerged. Half of participants followed a trajectory of sustained abstinence, meaning they reported almost no smoking during the year following delivery (see Figure). The other three trajectories consisted of individuals who resumed smoking during the first postpartum year. The largest of these groups (21% of the full sample) followed a trajectory of quick resumption – resuming smoking within 100 days after delivery. Thirteen percent of participants belonged to the delayed resumption group; they maintained abstinence for about six months and resumed smoking towards the end of the first postpartum year. The rest (16%) followed a trajectory of inconsistent smoking with multiple instances of smoking resumption followed by periods of abstinence during the year.
There were few factors that predicted trajectory group membership. Participants with more quit attempts, and those who smoked more cigarettes prior to quitting during pregnancy, were more likely to follow a trajectory of quick resumption compared to sustained abstinence.
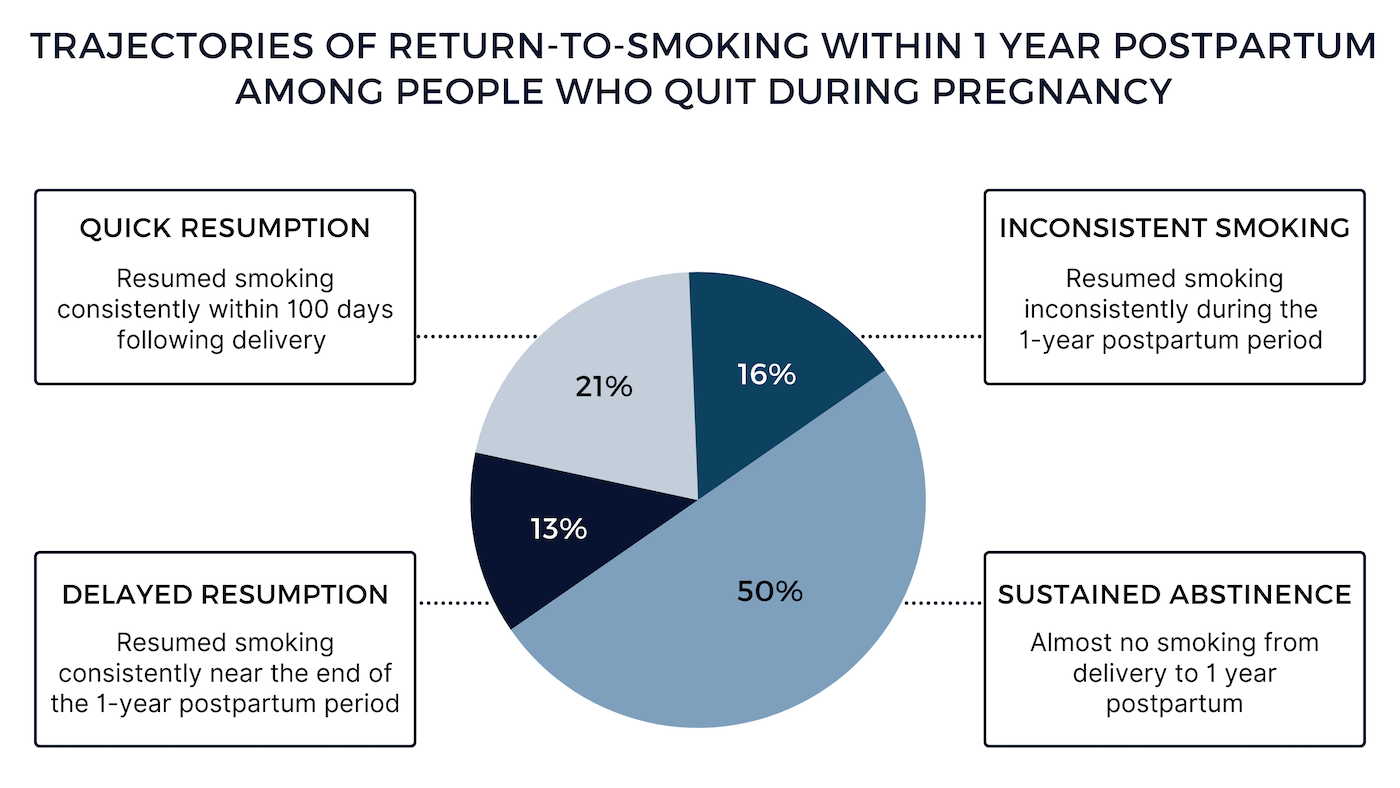
Figure. Four distinct trajectories of return-to-smoking from delivery to 1 year postpartum among people who quit smoking during pregnancy. Click image to enlarge.
Why do these findings matter?
Return-to-smoking during the postpartum period is a serious health concern. This study found that the three months following delivery is an especially critical time. Interventions to prevent smoking resumption should be offered during this time. Healthcare providers should consider assessing pregnant patients’ smoking history, particularly the number of previous quit attempts and number of cigarettes smoked per day, to identify those who might be at increased risk of quick resumption and who would benefit from targeted interventions immediately following delivery.
Every study has limitations. What are the limitations of this study?
Participants were enrolled in a randomized control trial on postpartum smoking resumption prevention and may have been more motivated to quit smoking and maintain abstinence during and after pregnancy. The study also took place in an urban area and participants were generally younger and of lower socioeconomic status. Therefore, findings might not be generalizable to other demographic groups (e.g., older individuals or those living in rural areas).
For more information:
SmokeFree offers tools and tips for quitting smoking while pregnant and maintaining abstinence from smoking tobacco after birth. The Centers for Disease Control and Prevention also provides research and tips about cigarettes and how to quit. For additional self-help tools, please visit the BASIS Addiction Resources page.
— Kira Landauer, MPH
What do you think? Please use the comment link below to provide feedback on this article.




