Peer recovery coaches (PRCs) are people in recovery who provide non-clinical coaching and support to peers who are seeking to initiate and maintain recovery from a substance use disorder (i.e., recoverees). PRCs are in a unique position to address smoking among individuals in addiction treatment, who experience higher smoking rates compared to the general population. This week, ASHES reviews a study by Joanna M. Streck and colleagues that examined how PRCs view and practice tobacco treatment in substance use disorder recovery coaching.
What was the research question?
What are PRC practices and attitudes towards tobacco treatment in substance use disorder recovery coaching?
What did the researchers do?
The researchers recruited PRCs from 12 substance use disorder treatment programs in a large Massachusetts-based healthcare system. Twenty-three PRCs completed an initial survey that asked about their smoking history, tobacco-related practices used with recoverees (e.g., smoking with recoverees), and attitudes about integrating tobacco treatment into their coaching (e.g., “peer recovery coaches should have a role in helping individuals in SUD treatment quit smoking”). A subset of participants (n = 20) completed a follow-up interview that assessed the reasons for PRCs’ tobacco-related practices and attitudes.
What did they find?
Half of the PRCs were former smokers and one-third were current smokers. PRCs engaged in both pro-smoking practices (e.g., accompanying recoverees outside to smoke) and pro-cessation practices (e.g., regularly asking recoverees about their cigarette smoking) (see Figure). The majority of PRCs considered smoking to be socially acceptable in substance use disorder treatment. PRCs generally believed that they should have a role in helping recoverees quit smoking, especially if they were former smokers themselves. However, PRCs generally agreed that addressing tobacco treatment during substance use disorder recovery coaching should only happen if the recoveree expresses interest and if it is part of their treatment goals. Lack of training in tobacco cessation practices and the need to address more immediate health needs, such as possible opioid overdose, were cited as reasons why some PRCs viewed smoking cessation as a low priority.
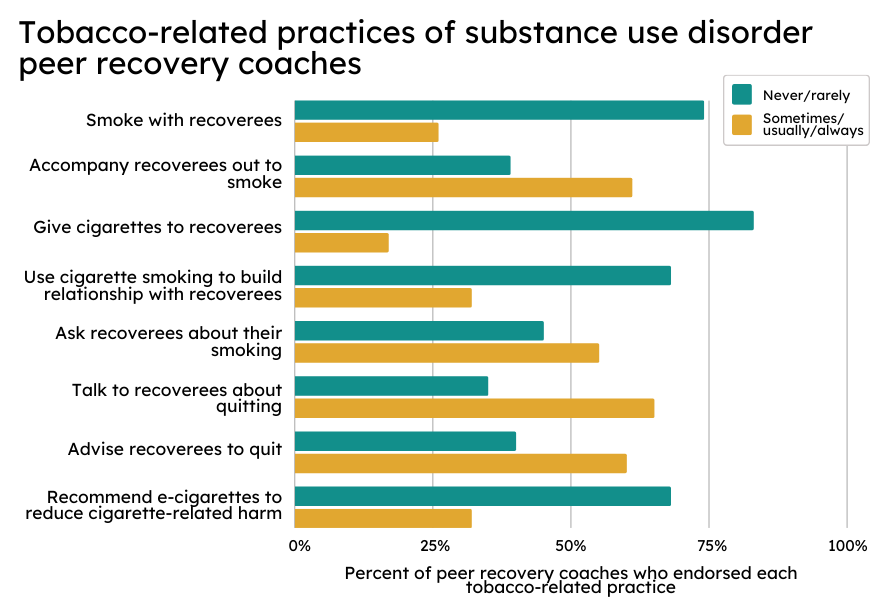
Figure. Tobacco-related practices endorsed by substance use disorder PRCs. Adapted from Streck et al. 2023. Click image to enlarge.
Why do these findings matter?
Cigarette smoking is associated with increased risk of return to substance use (i.e., relapse), making it important to address among individuals in addiction treatment. This study’s findings indicate there is potential feasibility in integrating tobacco treatment into recovery coaching for substance use disorders. Former smoker PRCs were the most committed to tobacco treatment during coaching and might be well equipped to administer tobacco cessation given their lived experience. Barriers to administering tobacco treatment among PRCs include lack of knowledge on this topic; PRC training curricula should cover how to support tobacco cessation for recoverees. Finally, smoking cessation guidelines recommend all individuals who smoke be offered smoking cessation services. This contrasts with the sentiment shared by PRCs that tobacco treatment only be offered to recoverees who express interest — a view that aligns with the tenets of patient-centered care in which recovery coaching is grounded. A framework for providing patient-centered smoking cessation guidelines should be developed for PRCs.
Every study has limitations. What are the limitations of this study?
Findings from this study might not be generalizable to other geographic areas or healthcare systems. Findings from this study are self-reported and might be subject to bias.
For more information:
SmokeFree offers tools and tips for quitting and maintaining abstinence from smoking tobacco. The Centers for Disease Control and Prevention also provides research and tips about cigarettes and how to quit. For additional self-help tools, please visit the BASIS Addiction Resources page.
— Kira Landauer, MPH
What do you think? Please use the comment link below to provide feedback on this article.