Many inpatient psychiatry units permit their patients to smoke; partially in response to patient advocacy groups, and partially in the hope that regular smoke breaks will help patients calm down and manage their symptoms (Lane et al., 2009). This stands in stark contrast to policies on other substances of abuse, such as alcohol and hard drugs, which are banned. There are very few clinical trials that have initiated tobacco interventions in this setting, and none have examined the effects of treating tobacco dependence on the recovery and psychological wellbeing of psychiatric inpatients. The current study recruited smokers from an acute inpatient psychiatric ward to participate in a randomized controlled trial of a smoking cessation intervention (Prochaska, S. E. Hall, Delucchi, & S. M. Hall, 2014).
Methods
- 224 smokers were recruited from an acute inpatient psychiatry unit that enforced a total ban on cigarettes. Hospital stays averaged 7.4 days (SD = 5.7; median = 6.0). Researchers randomized participants to one of two conditions:
- 140 people received treatment as usual (nicotine replacement therapy [NRT] during stay only)
- 94 people received nicotine replacement therapy plus a tobacco cessation intervention. The intervention included a computer-delivered intervention based on the Transtheoretical Model, an individualized report tailored to the individual’s stage of change, temptations and other processes of change related to tobacco, a 15-30 minute counseling session, continued NRT available after discharge, and a letter to the person’s primary health care provider requesting support with smoking cessation.
- Researchers assessed participants at baseline for demographic information, tobacco use history, nicotine dependence, depression, alcohol and drug use disorders, thoughts about abstinence, and position on a smoking readiness-to-change scale.
- At 3 and 6-month follow–up, researchers repeated the computerized intervention with the experimental group. At 3, 6, 12, and 18-month follow up, researchers assessed participants in both conditions for two main outcome measures:
- Past-week tobacco abstinence, as measured by the number of cigarettes, even a puff, or any form of tobacco used in the past week. Reported abstinence was verified using an air carbon monoxide smokerlyzer)
- Rehospitalization for psychiatric illness, as measured by patients’ responses, and then secondary confirmation with the electronic billing system
Results
- There were significant differences between the intervention and control condition (OR=3.39; 95% CI=1.32-8.72; p=.011) in abstinence rates modeled over 18 months.1 (See Figure 1 for a detailed breakdown of abstinence rates by time)
- The researchers ran a logistic regression with rehospitalization at any point during the 18-month trial as the dependent variable. Treatment condition was a significant predictor of re-hospitalization, as was psychosis, unstable housing, and previous hospitalization. Those who received the nicotine patch only were more likely to be re-hospitalized than those who received the tobacco intervention.
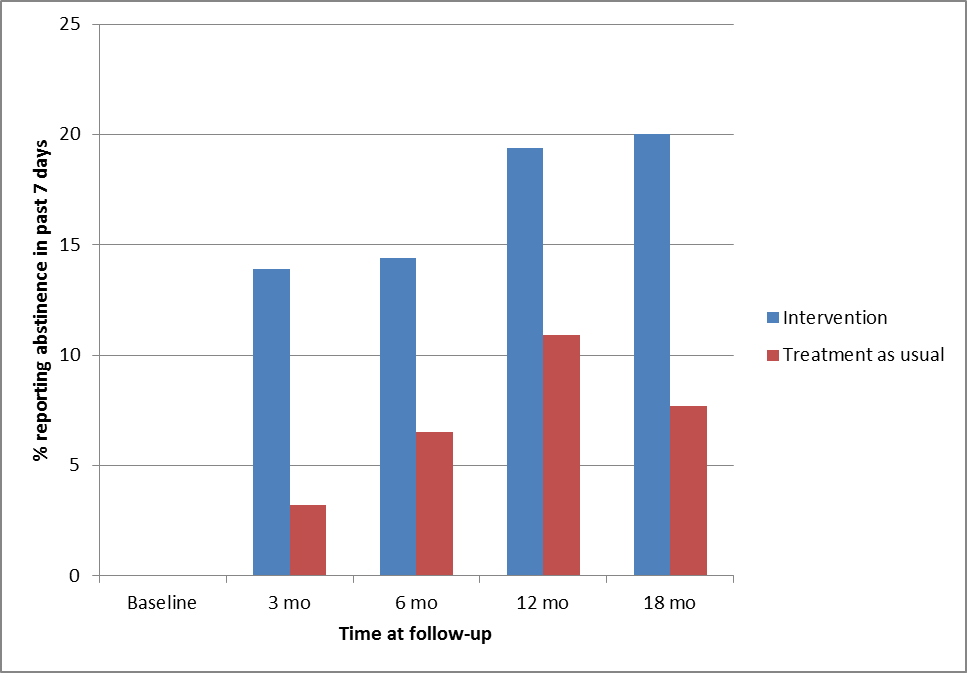
Figure. Tobacco abstinence rates by treatment condition over 18 months (adapted from Prochaska et al., 2014) Click image to enlarge.
Limitations
- It is possible that treatment as usual, which included a smoking ban, increased rehospitalization rates among psychiatric patients compared rates that might occur without intervention on a unit that allowed smoking.
- Participants in the intervention condition received not only an intervention during hospitalization, but also the option for continued NRT after hospitalization. As a result, it is not clear which aspect of the intervention led to the positive outcomes in this group.
Discussion
The results of this study indicate that tobacco cessation treatment for smokers who are in acute psychiatric hospital units might have positive effects on their smoking cessation when they leave the unit. Furthermore, the results indicate that tobacco cessation treatment with behavioral intervention might decrease the odds of rehospitalization. Future research ought to compare the effectiveness of inpatient psychiatric smoking bans with and without tobacco cessation interventions to permitting smoking in promoting positive psychiatric outcomes.
–Kat Belkin
References
Lane, J.G., Werdel, M.B., Schacht, L., Ortiz, G., Parks, J. (2009) Smoking policies and practices in state psychiatric facilities: survey results from 2008. National Assocation of State Mental Health Program Directors Research Institute, Inc; Alexandria, Virginia.
Prochaska, J.J., Hall, S.E., Delucchi, K., and Hall, S.M. (2014). Efficacy of initiating tobacco dependence treatment in inpatient psychiatry: A randomized controlled trial. American Journal of Public Health, 104(8), 1557-1565.
What do you think? Please use the comment link below to provide feedback on this article.
________________
1The effect of condition on abstinence rate remained significant when other baseline variables associated with abstinence were entered into the model. The reported comparisons assume that participants lost to follow-up remained smokers. However, the effect of condition on abstinence rate also remained significant when missing data were imputed.