People who experience substance-use disorders (SUD) also tend to experience a range of comorbid psychiatric conditions (e.g., Kessler et al., 1997). Some evidence suggests that the profile of comorbid conditions differs for men and women with SUD (e.g., Kessler et al., 1997). However, past estimates of sex-specific comorbid associations have not been adjusted for sociodemographic characteristics and the presence of other co-occurring psychiatric conditions. This week’s STASH reviews a study that examines sex-specific comorbid associations with SUD while controlling for these additional variables (Goldstein, Dawson, Chou, & Grant, 2012).
Methods
- The researchers used data from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), which gathered data on SUD, other psychiatric conditions, and sociodemographic characteristics using face-to-face interviews during 2004-2005 (n=34,653) (Grant, Kaplan, Moore, & Kimball, 2007).
- Interviewers assessed SUD and other psychiatric conditions using the Alcohol Use Disorders and Associated Disabilities Interview Schedule-DSM-IV version (AUDADIS-IV; Grant, Dawson, & Hasin, 2004). The AUDADIS-IV measures DSM-IV criteria for abuse and dependence of 10 drug categories. All conditions were measured on a lifetime basis.
- Goldstein and colleagues used sex-specific multivariate logistic regressions to estimate associations of drug use disorders with other psychiatric disorders1, first controlling only for sociodemographic characteristics and then controlling for both sociodemographic characteristics and all other Axis I and II disorders.2
Results
- Men were more likely than women to report drug abuse and dependence (both χ2 (1) > 36; both p < .001).
- In the analysis controlling for only sociodemographic characteristics, drug abuse was positively associated with all examined psychiatric disorders except bipolar II (risk only higher among women) and dependent personality disorder (risk only higher among men).
- The patterns between men and women were largely similar; the only odds ratios that differed between men and women were for any alcohol use disorder and nicotine dependence (both higher among women).
- As displayed in Figure 1, when researchers also controlled for the presence of other Axis I and II disorders, drug use disorders remained significantly and positively associated in both sexes with any mood disorder, bipolar I disorder, any alcohol use disorder, alcohol abuse, nicotine dependence, any personality disorder, and antisocial personality disorder; in men with ADHD and major depression; and in women with borderline personality disorder.
- Odds ratios differed significantly between men and women only for bipolar I disorder and alcohol abuse (risk higher among women) and any personality disorder (risk higher among men).
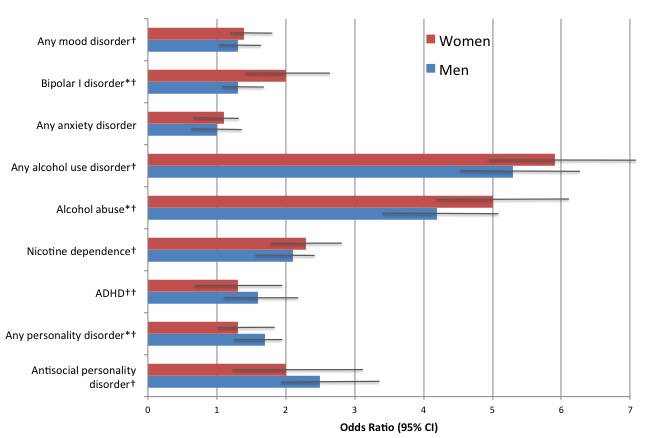
Figure. Odds ratios (95% confidence intervals) for selected associations between drug use disorders and other psychiatric disorders among NESARC respondents, as a function of sex. Adapted from Goldstein et al. (2012). *Odds ratios are significantly different (at p < .05) between women and men. †Odds ratios are significantly different (at p < .05) than 1 for both women and men. ††Odds ratio is significantly different (at p < .05) than 1 for men only. Click image to enlarge.
Limitations
- Because this study used a cross-sectional design, it is impossible to identify causal mechanisms, such as a mood disorder causing drug abuse.
- Although the NESARC used strict confidentiality guarantees, self-reports of drug abuse—like self-reports of all stigmatized behaviors–are susceptible to self-presentation biases.
Conclusions
This study adds to a growing body of evidence indicating that people who experience drug abuse are at higher risk for other psychiatric disorders. This pattern highlights the need for careful assessment and integrated treatment of mental health disorders during SUD treatment. A novel contribution of this study is the adjustment for sociodemographic characteristics and other psychiatric conditions. With this adjustment, the associations between SUD and other psychiatric conditions are weaker than those previously reported (Kessler et al., 1997), potentially because much of the comorbidity between SUD and other specific psychiatric conditions reflects high rates of the co-occurrence of other conditions. When this artifact is considered, gender differences in the profile of comorbid conditions tend to fall away.
–Heather Gray
What do you think? Please use the comment link below to provide feedback on this article.
References
Goldstein, R. B., Dawson, D. A., Chou, S. P., & Grant, B. F. (2012). Sex differences in prevalence and comorbidity of alcohol and drug use disorders: results from wave 2 of the national epidemiologic survey on alcohol and related conditions. Journal of Studies on Alcohol and Drugs, 73(6), 938-950.
Grant, B. F., Dawson, D. A., & Hasin, D. (2004). The Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions Alcohol Use Disorders and Associated Disabilities Interview Schedule-DSM-IV Version. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism.
Grant, B. F., Kaplan, K., Moore, T., & Kimball, J. (2007). 2004-2005 Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions: Source and accuracy statement. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism.
Kessler, R. C., Crum, R. M., Warner, L. A., Nelson, C. B., Schulenberg, J., & Anthony, J. C. (1997). Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Archives of General Psychiatry, 54, 313-321.
________________
[1] The researchers performed the same set of analyses for alcohol use disorders, but we are not reporting those results here.
[2] For example, the fully adjusted model exploring comorbidity between drug abuse and social phobia adjusted for sociodemographic characteristics plus any mood disorder, any anxiety disorder except social phobia, any alcohol use disorder, nicotine dependence, ADHD, and any personality disorder.