The number of opioid overdoses in the United States has dramatically increased over the past decade. Buprenorphine and other medications for opioid use disorder are effective at reducing cravings and reducing withdrawal symptoms. Unfortunately, prescribing rates for these medications are significantly lower for marginalized populations, such as people experiencing housing instability, than they are for more privileged individuals. This disparity results in marginalized individuals being at a much bigger risk of opioid overdose. As a first step toward understanding some of the access challenges that people experiencing homelessness have, Michael Hsu and colleagues conducted qualitative interviews with individuals living near the Boston Public Health Commission Engagement Center.
What was the research question?
What challenges do people experiencing homelessness with opioid use disorder have related to accessing opioid medications?
What did the researchers do?
The researchers conducted semi-structured interviews with people living near the Boston Public Health Commission Engagement Center. They used both open- and close-ended questions that probed the experiences that participants had related to accessing opioid use treatment. After completing interviews, the researchers conducted thematic analysis, which involves closely analyzing participants’ answers to questions to identify themes. In total, the researchers interviewed 28 people. Participants were, on average, 44-years-old, mostly male (64%) and many were not actively receiving treatment (54%). Their sample was racially and ethnically diverse with 36% of participants identifying as Black, 36% identifying as White, 21% identifying as Latine, and 7% identifying as American Indian.
What did they find?
The researchers identified four overarching themes related to difficulties accessing treatment for opioid use disorder: (1) acceptability, (2) availability, (3) accommodation, and (4) accessibility (see Figure).
- Acceptability themes included participants’ fears related to experiencing negative side effects from medications for opioid use disorder, as well as fear of addiction hopping, having poor past experiences in treatment clinics, and experiencing stigma toward opioid medication. For example, one participant stated, “I’m worried about my bipolar and stuff like that. I don’t know how I would react to meds, how meds could affect my mental illness.”
- Availability challenges involved having fewer treatment opportunities due to the COVID-19 pandemic. Women specifically also noted that they also had fewer treatment beds available than men. One of their participants stated, “I’ve called detox places and I can’t even get beds anymore during the pandemic. Males get beds easier.”
- Participants also noted that their treatment providers did not make accommodations for their life circumstances. For instance, some participants expressed difficulty adhering to rigid methadone treatment requirements while others said that they could not replace medications that were either lost or stolen. One participant noted, “Taking methadone sucked. I had to revolve my life around it. I had to make sure I got up every morning to go. I have a newborn child. It’s hard.”
- Finally, in terms of accessibility, participants stated that they could not always get reliable transportation to treatment centers with one of their participants stating, “Sometimes it’s hard to get into detox because if you don’t have a ride, you can’t get there.”
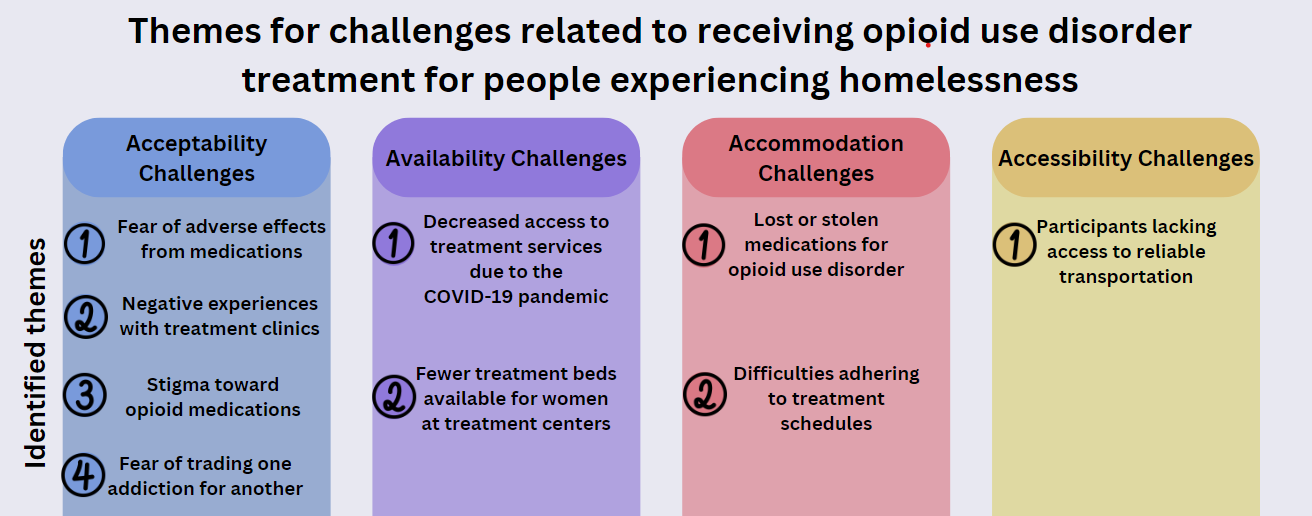
Figure. This Figure, adapted from Hsu and colleagues, depicts the themes that the researchers identified related to the challenges that participants faced when trying to receive treatment for opioid use disorder. Click image to enlarge.
Why do these findings matter?
Several prominent barriers impede individuals experiencing homelessness from accessing treatment for opioid use disorder, including the inability to physically access treatment centers. In particular, participants noted that they could not reliably access transportation to get to treatment centers. This is important because it indicates that some people might be interested in receiving treatment but are unable to because they cannot afford to travel to a treatment facility. In turn, this exacerbates health inequalities as individuals with more available resources are able to receive treatment while those without the financial means cannot. To help counteract this, treatment centers should try to issue passes or vouchers to cover public transportation costs. Additionally, participants noted that they were afraid of trading one addiction for another. This indicates that there are misconceptions related to medications for opioid use disorder and that efforts are needed to clarify these misinformed beliefs among people with addiction. Some recent research has noted that even healthcare providers often possess misinformed beliefs related to these medications, which suggests a comprehensive effort is needed to correct these falsehoods.
Every study has limitations. What are the limitations in this study?
The results might not extend beyond this study’s context. For example, people experiencing homelessness in other cities or in more rural environments, or people who are marginalized in other ways, such as by disabilities or previous incarceration, might experience other difficulties related to accessing treatment for opioid use disorder. Another limitation of the study is that the researchers only examined the perspectives of patients. Healthcare providers often hold stigma against patients experiencing opioid use disorders and other kinds of addiction, and those attitudes could impede patients’ ability to receive and benefit from treatment. Future research should work to assess new ways to promote more empathetic caregiving.
For more information:
If you are worried that you or someone you know is experiencing addiction, the SAMHSA National Helpline is a free treatment and information service available 24/7. For more details about addiction, visit our Addiction Resources page.
— Seth McCullock, PhD
What do you think? Please use the comment link below to provide feedback on this article.





steven gilboard February 13, 2024
EXCELLENT AND RIGHT ON THE MARK