Although overall smoking prevalence has decreased among U.S. adults in the past few decades, this decrease tends to be smaller in rural and Appalachian areas. This is partly due to the Appalachian region being characterized by tobacco agriculture, poverty, and limited access to healthcare. People in rural areas are also more likely to experience social vulnerability, or susceptibility to the negative effects of various social and environmental factors such as unemployment and lack of transportation access. Might social vulnerability be related to smoking patterns in Appalachian regions? This week, ASHES reviews a study by Asal Pilehvari and colleagues that examined this question.
What was the research question?
Do rural counties, Appalachian counties, and counties with greater social vulnerability in Virginia have a higher smoking prevalence?
What did the researchers do?
The researchers used data from the Virginia Behavioral Risk Factor Surveillance System to estimate county-level cigarette smoking prevalence. They designated adults who had a current smoking frequency of “every day” or “some days” and had smoked more than 100 cigarettes in their lifetime as smokers. The researchers distinguished rural and urban counties using the Department of Agriculture’s Rural-Urban Continuum Codes and distinguished Appalachian and non-Appalachian counties using the Appalachian Regional Commission database. They determined each county’s level of social vulnerability using the CDC’s Social Vulnerability Index (SVI). They used independent sample t-tests to compare average smoking prevalence rates between counties based on rurality and Appalachian status and used multivariate regression to analyze the impact of social vulnerability on smoking prevalence.
What did they find?
Smoking prevalence was higher in rural counties (19.9%) compared to urban counties (13.2%, see Figure) and higher in Appalachian counties (20.9%) compared to non-Appalachian counties (13.4%). Average SVI score, which ranges from 0 to 1, was higher in rural counties (0.63) compared to urban counties (0.40) and higher in Appalachian counties (0.51) compared to non-Appalachian counties (0.50). Greater social vulnerability was significantly associated with increased smoking prevalence, particularly in rural Appalachian counties.
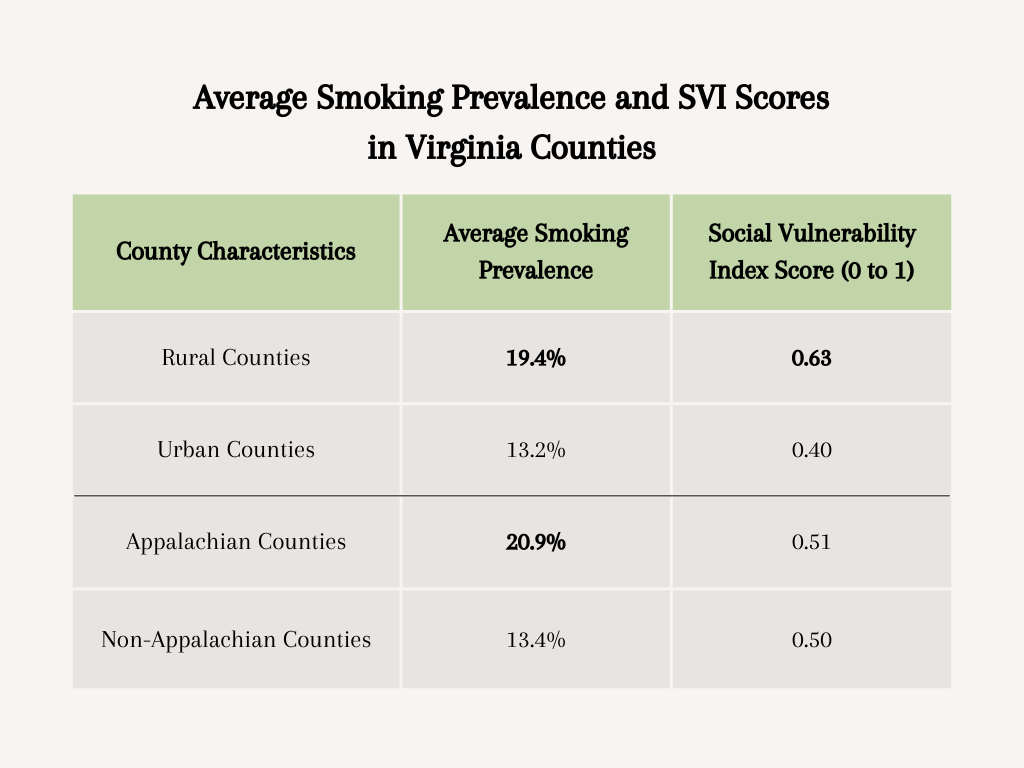
Figure. Average smoking prevalence and SVI scores of Virginia counties by rurality and Appalachian status. Statistically significant differences are shown in bold. Click image to enlarge.
Why do these findings matter?
Smoking prevalence among adults in rural and Appalachian areas is disproportionately high, which could have broader public health implications. Specifically, a variety of factors such as a shortage of healthcare providers, poverty, and pro-tobacco culture might contribute to greater cigarette use in these regions. Thus, it is important to implement targeted interventions to reduce cigarette use and general health disparities in these areas. Examples of interventions might include relevant prevention programs to reduce smoking initiation in adolescents, increasing access to anti-tobacco campaigns, and expanding policies to reduce secondhand smoke exposure.
Every study has limitations. What are the limitations in this study?
This study examined smoking prevalence in Virginia, so the findings might not be generalizable to residents in other geographic regions. Additionally, the researchers used SVI levels to measure overall social vulnerability, but did not examine specific social and environmental factors (e.g., race, education, socioeconomic status) that are likely to affect smoking patterns.
For more information:
SmokeFree offers tools and tips for quitting and maintaining abstinence from smoking tobacco. The Centers for Disease Control and Prevention also provides research and tips about cigarettes and how to quit. For additional self-help tools, please visit The BASIS Addiction Resources page.
— Annette Siu
What do you think? Please use the comment link below to provide feedback on this article.




