Healthcare providers are optimally positioned to help patients quit smoking through the delivery of smoking cessation care. Providers can help patients stop smoking by advising them to quit, providing brief counseling, prescribing medication, and connecting patients with resources such as a quitline. However, there are numerous barriers that might impact implementation of smoking cessation care. This week, ASHES reviews a study by Eline Meijer and Niels H. Chavannes that examined healthcare providers’ perceptions of smokers’ responsibility for smoking and how it relates to provider views on barriers to and the implementation of smoking cessation care.
What were the research questions?
Do different subgroups of healthcare providers exist with regards to their perceptions of smokers’ responsibility for smoking? Do these subgroups differ regarding views on barriers to, sense of responsibility for, and experiences with the implementation of smoking cessation care?
What did the researchers do?
Five hundred and seventy healthcare providers (i.e., physicians, dentists, dental hygienists, and midwives) in the Netherlands completed an online survey about their perceptions of smokers’ responsibility for smoking. The researchers conducted a latent class analysis to determine which, and how many, subgroups of healthcare providers exist regarding views on smoking responsibility. Survey respondents also reported on perceived barriers to, sense of responsibility for, and experiences with the implementation of smoking cessation care. The researchers examined whether and how these perceptions differed between the subgroups of healthcare providers.
What did they find?
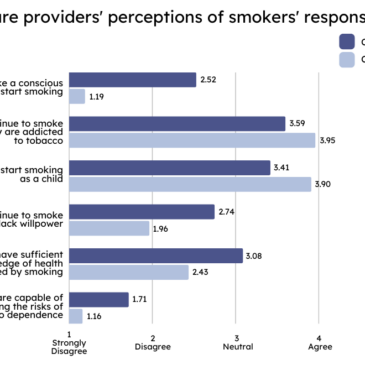
Latent class analysis identified two subgroups of healthcare providers. The majority (77%) of healthcare providers fell into a group which was more likely than the other group to hold smokers accountable for their smoking (Class 1). The rest (23%) were more likely than the other to believe that people smoke because of factors like addiction or smoking initiation at a young age when one cannot fully recognize the potential consequences of smoking (Class 2). Class 2 providers were more likely than Class 1 providers to disagree with the statements such as “smoking initiation is a conscious choice” and “smokers continue to smoke because they lack willpower” (see Figure).
Class 1 providers were generally younger and had fewer years of working experience than Class 2 providers. Membership was related to the provider’s smoking status; ex-smokers were more likely to belong to Class 2. Providers in Class 1 experienced more barriers to smoking cessation care, including patient dishonesty about smoking and concerns about harming the patient-provider relationship. The two classes were equally likely to believe that healthcare providers have a responsibility to provide smoking cessation care. Providers in Class 1 provided smoking cessation advice and assessed motivation to quit among fewer patients who were smokers than providers in Class 2.
Figure. Healthcare providers’ perceptions of smokers’ responsibility for smoking. The graph depicts the mean rating (on a Likert scale from 1 – Strongly disagree to 5 – Strongly agree) of agreement with each statement for both subgroups of healthcare providers. Click image to enlarge.
Why do these findings matter?
This study found that healthcare providers’ perceptions of smokers’ responsibility for smoking are related to their views on barriers to, and the implementation of, smoking cessation care. Improving smoking cessation care might require different approaches based on healthcare provider perceptions of smokers’ responsibility. This study found that providers who are ex-smokers are less likely to hold smokers personally accountable for their smoking. These providers could share their own experiences quitting tobacco with their peers to address the misconceptions about smokers’ responsibility. Further, healthcare provider training programs might place more focus on the factors beyond the smoker’s control that can contribute to smoking.
Every study has limitations. What are the limitations of this study?
Findings from this study may not be generalizable to other groups of healthcare providers not included in this study (e.g., nurses) or to settings outside of the Netherlands. Causality cannot be determined because this study used a cross-sectional design. In other words, we cannot determine whether perceptions of smokers’ responsibility affected perceived barriers to smoking cessation care, or vice versa.
For more information:
SmokeFree offers tools and tips for quitting and maintaining abstinence from smoking tobacco. The Centers for Disease Control and Prevention also provides research and tips about cigarettes and how to quit. For additional self-help tools, please visit the BASIS Addiction Resources page.
— Kira Landauer, MPH
What do you think? Please use the comment link below to provide feedback on this article.