People who stop using illicit substances might turn to alcohol as a kind of “addiction hopping.” Although alcohol consumption is linked to an increased risk of relapse to the initial substance use disorder (SUD), there isn’t much research about the rate, correlates, and consequences of alcohol use among adults who have successfully recovered from SUDs. This week, The DRAM reviews a study by Taeho Greg Rhee and Robert Rosenheck that explored these issues.
What were the research questions?
How common is it for people to develop an alcohol use disorder (AUD) after recovering from a SUD, and what are the characteristics of those who do? What is the impact of AUD on the quality of life among these adults?
What did the researchers do?
The researchers used data from the 2013 National Epidemiologic Survey on Alcohol and Related Conditions Wave III (NESARC-III). This study’s sample only included adults who met criteria for previous, but not current,1 SUDs (e.g., opioid use disorder, stimulant use disorder)–in other words, people who reported having recovered from a SUD. The researchers split the 2,061 adults into three categories: those who currently met criteria for AUD, those who met criteria for lifetime AUD but not current AUD (i.e., they had recovered from AUD), and those with no history of AUD. They then looked at sociodemographic characteristics, other psychiatric and medical conditions, and health-related quality of life indicators.
Rhee and Rosenheck then used logistic regression analysis to determine which of the sociodemographic and health-related quality of life correlates were associated with currently having a AUD, versus never having had or having already recovered from AUD.
What did they find?
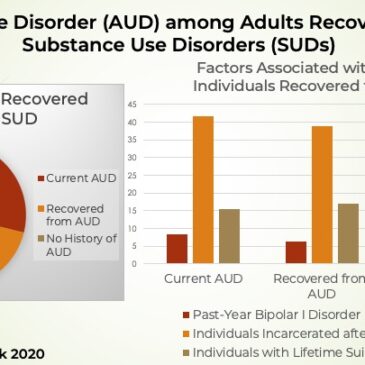
Of the 2,061 adults who had recovered from a SUD, 29% met criteria for current AUD, 48% had recovered from AUD, and 23% had no history of AUD.
What distinguished the people who were currently experiencing AUD? First, they were more likely to also have a medical condition such as diabetes or hypertension, compared to those in the other two groups. They reported worse mental health, compared to the other two groups. Also, compared to those with no history of AUD, they were 1.8 times more likely to have been incarcerated, 4.2 times more likely to have bipolar I disorder, and 1.53 to have made a suicide attempt.
In terms of demographic characteristics, people in recovery from a SUD who currently had an AUD were more likely than those who recovered from or never experienced an AUD to be divorced/separated/widowed/partnered rather than married, and to live in urban areas. They were also younger.
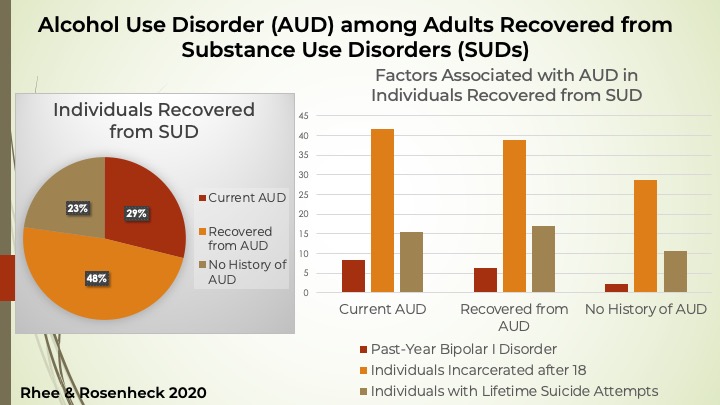
Figure. This figure shows the percentages of individuals recovered from SUD in each group and a few factors that were positively associated with currently having an AUD. Click image to enlarge.
Why do these findings matter?
Essentially, these findings tell us that many people who recover from an addiction to cocaine, opioids, stimulants, or other substances go on to experience a problem with drinking. This is important for SUD treatment providers to know — it suggests that SUD treatment should prepare the client for the potential for “addiction hopping” and how to avoid it. Particularly when working with a client suffering from AUD, clinicians should address any other psychiatric conditions (e.g., bipolar disorder) or life experiences (e.g., lifetime incarceration or suicide attempts) that could complicate the treatment and recovery process.
Every study has limitations. What are the limitations in this study?
Although the NESARC-III is a nationally representative sample, it did exclude anyone who is currently on active duty in the military, homeless, incarcerated, or institutionalized elsewhere. This can limit the ability to generalize the findings of this study. Additionally, this data was taken at a single time point; therefore, the researchers were unable to explore trends over time.
For more information:
The National Institute on Alcohol Abuse and Alcoholism has tips and resources for people struggling with problem drinking. For drinking self-help tools, please visit The BASIS Addiction Resources page.
Health professionals and addiction specialists have been increasingly focused on mental health as it pertains to COVID-19. They have assembled substance use resources specific to COVID-19-related concerns, as well as resources on alcohol use in general, which can be found on the National Institute on Drug Abuse and Centers for Disease Control and Prevention websites.
— Karen Amichia
What do you think? Please use the comment link below to provide feedback on this article.
________________
[1] In this wave of the study, the Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5) was used to find lifetime psychiatric and substance use disorders using DSM-5 criteria. The researchers defined “current AUD” as meeting criteria for AUD at any time in the previous twelve months.