Problem gambling often goes undetected and untreated. However, many individuals experiencing problem gambling seek treatment for other mental health concerns that often co-occur with gambling problems (e.g., affective disorders, psychotic disorders, substance use disorders). Clinicians – including mental health practitioners – are aptly positioned to identify and respond to problem gambling, although screening is infrequent in treatment settings. This week, The WAGER reviews a study by Victoria Manning and colleagues that examined mental health clinicians’ attitudes and behaviors toward identifying and responding to problem gambling.
What were the research questions?
How do mental health clinicians screen for and respond to problem gambling? What attitudes do mental health clinicians have toward problem gambling?
What did the researchers do?
The researchers recruited 281 mental health clinicians (e.g., nurses, medical staff, psychologists, social workers) from a range of adult mental health service and treatment sites throughout Victoria, Australia. The participants completed a self-report questionnaire that assessed knowledge of and attitudes towards problem gambling – including screening and assessment. Clinicians also answered questions that assessed their behaviors related to screening, referral, and treatment of problem gambling. The researchers analyzed and compared the responses using descriptive statistics.
What did they find?
Only 12.5% of clinicians reported ever being trained in screening and responding to problem gambling. Less than half of participants indicated they understood the causes and/or factors that maintain problem gambling and most were unaware of available problem gambling screening and assessment tools.
The majority of participants were willing to address problem gambling and felt that a brief problem gambling screen would be a useful part of their routine clinical practice. However, many felt they had insufficient time to screen for problem gambling and believed they had other more important issues to address (see Figure). Only 16% of clinicians reported that they often or almost always screened for problem gambling. Of those who did screen, most did so informally; only 2% reported using a standardized problem gambling screening tool.
Referrals to specialty problem gambling treatment occurred infrequently; only 11.7% of clinicians referred patients to needed services often or almost always. Rather, three-quarters of clinicians provided problem gambling treatment themselves. However, most (76.1%) were not confident or only somewhat confident in their ability to treat problem gambling and reported having a limited understanding of treatment options and available problem gambling services and resources.
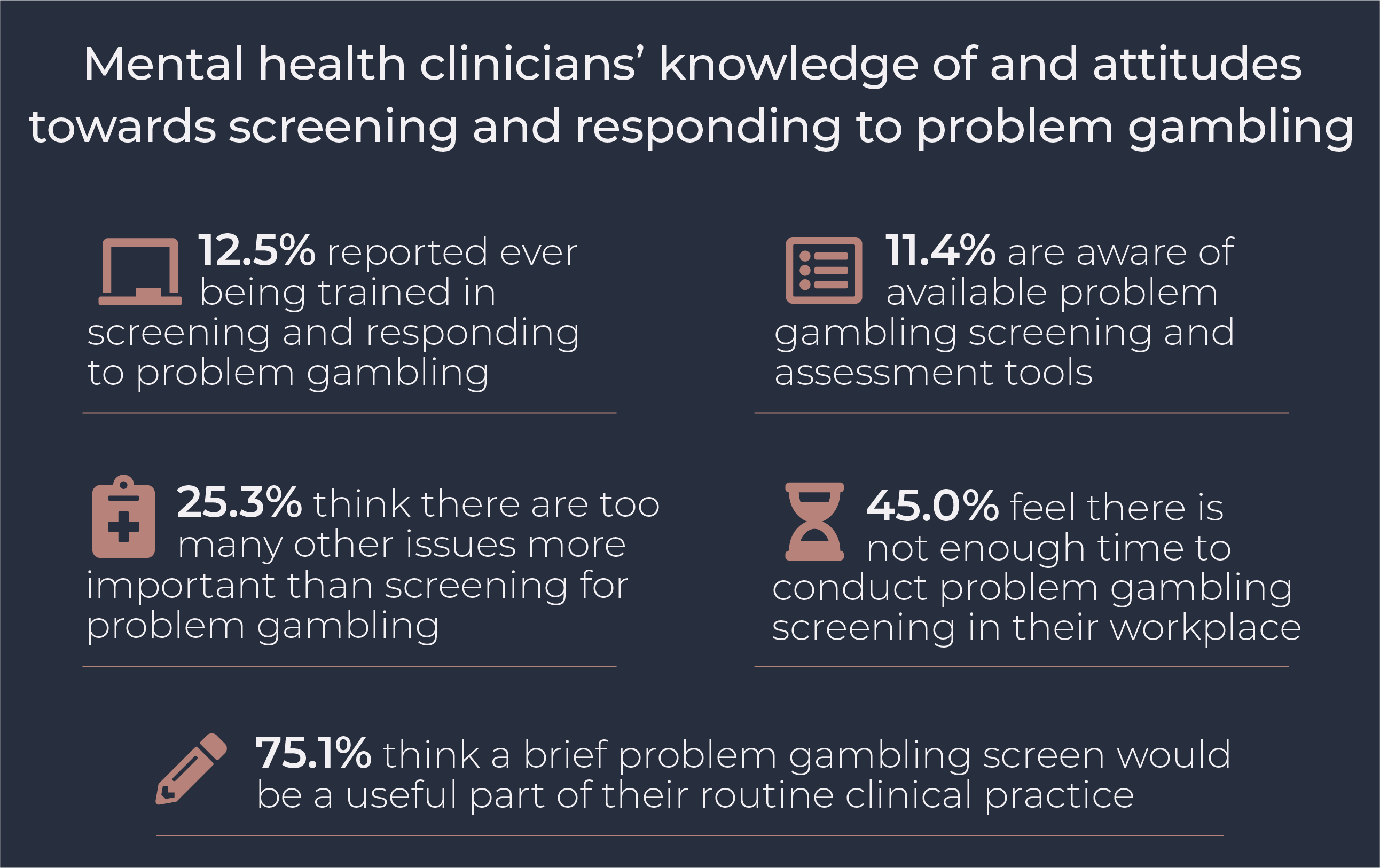
Figure. Mental health clinicians’ self-reported knowledge of and attitudes towards screening and responding to problem gambling in clinical practice. Click image to enlarge.
Why do these findings matter?
Routine screening for problem gambling in community mental health settings is an important means to detect and respond to gambling concerns among populations with elevated risk of comorbid mental health concerns and problem gambling. Mental health practices should consider universally screening all clients for problem gambling as part of routine clinical practice with the use of a brief screening tool. Low rates of problem gambling training indicate the need for increased education for mental health clinicians. Training opportunities should focus on clinician knowledge and skills related to understanding, identifying, and responding to problem gambling. Undergraduate and postgraduate training programs for mental health clinicians should consider including a requirement related to problem gambling education.
Every study has limitations. What are the limitations of this study?
Findings from this study may not be generalizable to other geographic locations (e.g., the United States) or clinician populations (e.g., non-mental health practitioners). Clinicians who chose to participate may have had greater interest in problem gambling, introducing the possibility of self-selection bias.
For more information:
Do you think you or someone you know has a gambling problem? Visit the National Council on Problem Gambling for screening tools and resources. For additional resources, including gambling and self-help tools, please feel free to visit The BASIS Addiction Resources page.
— Kira Landauer, MPH
What do you think? Please use the comment link below to provide feedback on this article.




Craig R. Johnson February 20, 2021
I consistently work with my colleagues who are mental health providers to screen patients for Gambling Disorder and we have, as a practice, increased awareness. There are only a very few Gambling Treatment providers in Minnesota (out of thousands of providers both for mental health and SUD) there are only 19 state certified gambling treatment providers. But the need is greater. I do periodic surveys of the SUD clients in out clinic, and find on average, about 30% of those patients will endorse at least one and often three of the questions on the Brief Biosocial Gambling Screen, but have not addressed Gambling Disorder as a co-occurring issue.