E-cigarettes have gained popularity, in part for their perceived role in helping smokers transition away from smoking cigarettes, which are likely more harmful. But health experts, such as Dr. John Blaha, worry that e-cigarettes will hook adolescents on nicotine, eventually leading to tobacco use: “It’s one thing if you convert from cigarette smoking to vaping. It’s quite another thing to start up nicotine use with vaping. And, it often leads to using traditional tobacco products down the road.” The ‘gateway hypothesis’ that using relatively less harmful substances encourages engagement with more dangerous substances has a long history. The ‘common liabilities hypothesis’ instead proposes that factors such as genes and peer substance use predispose some individuals to consume a variety of addictive substances. In this edition of STASH, we review a meta-analysis by Gary Chan and colleagues of longitudinal studies that estimate the effect of earlier e-cigarette use on later tobacco smoking while controlling for common liabilities.
What were the research questions?
Do studies show that e-cigarette use leads to cigarette smoking, even after accounting for common liabilities? To what extent are existing studies limited by inadequate controls, publication bias, and participant drop-out?
What did the researchers do?
The authors identified 11 prospective studies on the effect of earlier e-cigarette use on later tobacco cigarette use. The authors regarded studies as having adequately accounted for common liabilities to the extent that they controlled for six ‘key common liabilities’: associating with smoking peers, having family members who smoke, school commitment, alcohol and other substance use, intentions to smoke, and delinquent behavior.
What did they find?
Averaging the results of each study (weighted by their sample size) revealed that the odds of initiating cigarette smoking was 4.31 times higher for participants who had used e-cigarettes compared to participants who had not been using e-cigarettes. However, after adjusting for common liabilities, the odds were only 2.93 times higher. Even this adjusted estimate may be too high for three reasons. First, only two studies controlled for more than half of the key common liabilities. Second, the median rate of dropping out of the study before the follow-up was 30%, and participants with common liability risk factors were especially likely to drop-out. Finally, studies with smaller samples found larger effects, which researchers often interpret as evidence of publication bias (i.e. bias against studies that are consistent with the null hypothesis).
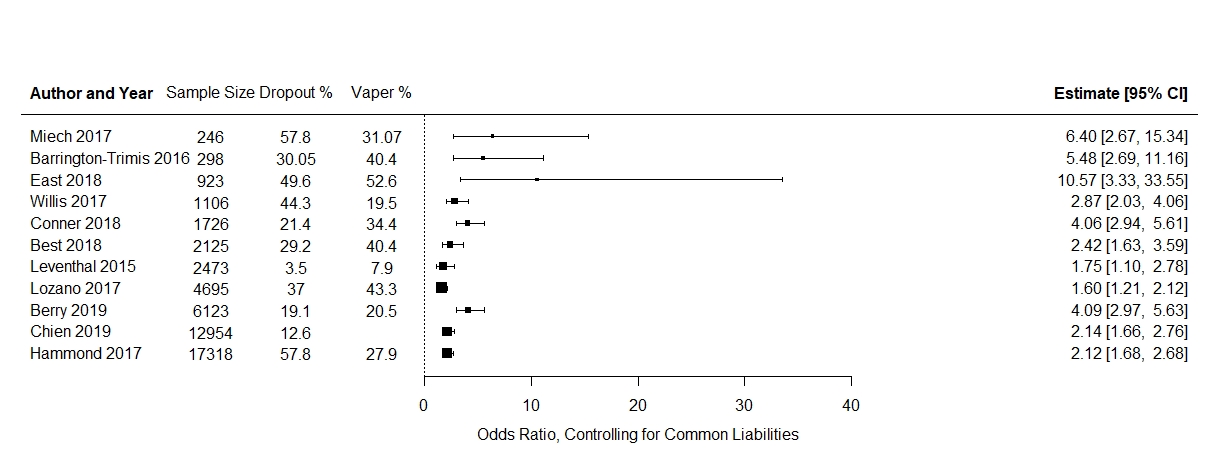
Figure. Each study is represented by a square representing the odds ratio of cigarette smoking initiation after vaping vs. not vaping at an earlier time-point, after controlling for common liabilities. The size of the square corresponds to the size of the study. The bands around the squares are 95% confidence intervals. Click image to enlarge.
Why do these findings matter?
The gateway hypothesis will not be definitively confirmed or rejected until all researchers control for all key confounds and adequately account for systematic differences between participants who drop out of longitudinal studies and those who remain in them. Until then, it is reasonable to speculate that the relationship between earlier e-cigarette use and later cigarette smoking among adolescents is partially causal and partially due to common liabilities. Whether further regulations on vaping would benefit society as a whole depends on the number of people who would have died prematurely or gotten sick from cigarette smoking but for the availability of e-cigarettes and the number of people who will die from becoming addicted to cigarettes via exposure to e-cigarettes, both of which are currently unknown.
Every study has limitations. What are the limitations of the study?
Many of the controls included in studies might be imperfect substitutes for the common liabilities that they represent. For instance, whether participants have a parent who smokes was used as a proxy for genetic vulnerabilities to substance use. This is an imprecise substitute because a parent could have a genetic predisposition towards smoking even if he or she does not actually smoke. Also, the authors were not able to explain the wide variability in findings across studies, which could be due to differing lengths of follow-up, samples coming from different countries, and non-representative sampling within countries.
For more information:
If you are worried that you or someone you know is experiencing addiction, the SAMHSA National Helpline is a free treatment and information service available 24/7. For more details about addiction, visit our Addiction Resources page.
— William McAuliffe, PhD
What do you think? Please use the comment link below to provide feedback on this article.