As we cope with the largest opioid epidemic in U.S. history, many are wondering whether the pain-relieving effects of marijuana could reduce or prevent opioid use disorder. While well-known past studies have found that states with legalized medical marijuana report fewer annual deaths from opioid overdoses than states without, research has not specifically addressed whether individuals who use marijuana are more likely to develop problems with opioids. This week, STASH reviews a 2017 study by Mark Olfson and colleagues investigating this relationship.
What was the research question?
Is marijuana use associated with increased risk of nonmedical prescription opioid use and opioid use disorder?
What did the researchers do?
The researchers examined data from 34,653 American adults who participated in wave 1 (2001-2002) and wave 2 (2004-2005) of the National Epidemiological Survey on Alcohol and Related Conditions (NESARC). The NESARC uses structured interviews to measure past-year frequency of marijuana use, medical and nonmedical1 prescription opioid use, symptoms of cannabis use disorder, and general pain level. The researchers used logistic regression to assess whether past-year marijuana use at wave 1 was related to incident nonmedical prescription opioid use and opioid use disorder at wave 2.2
What did they find?
The researchers restricted their focus to participants who reported that they had no nonmedical opioid use at wave 1. Those who used marijuana at wave 1 were significantly more likely to report nonmedical prescription opioid use at wave 2. Similarly, marijuana users at wave 1 were significantly more likely than non-users to later develop an incident opioid use disorder. Then, researchers focused on two subsets of participants: those who used marijuana but did not experience cannabis use disorder at wave 1, and those who used marijuana and reported moderate to severe pain at wave 1. Both of these groups were more likely to report incident nonmedical prescription opioid use, compared to those who did not use marijuana at wave 1 (see figure).
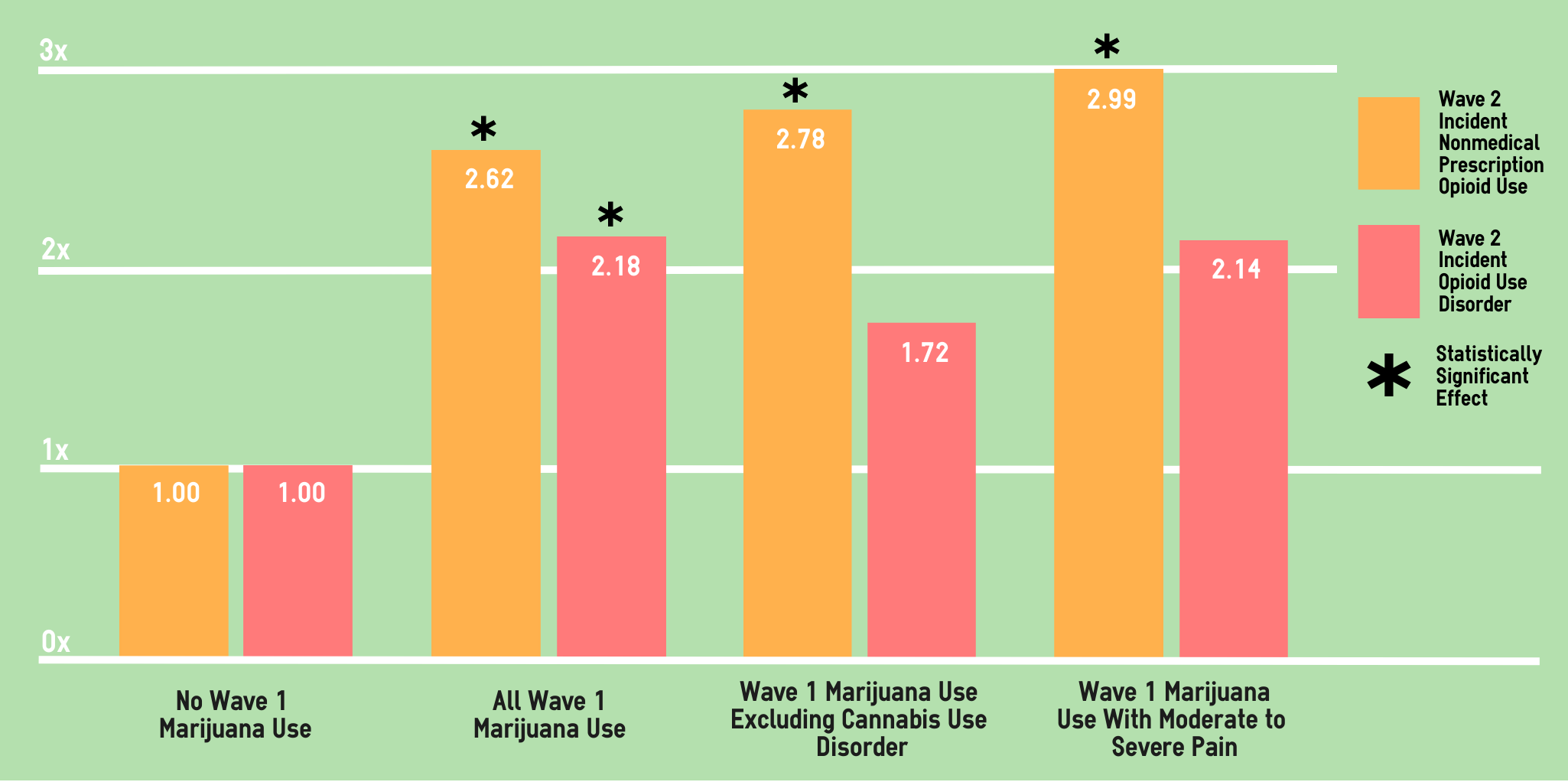
Figure. Adjusted Odds Ratios for the relationship between marijuana use patterns at wave 1 and incident prescription opioid use (orange bars) and opioid use disorder (pink bars) at wave 2. Participants who reported no wave 1 marijuana use served as the referent group. Click image to enlarge.
Why do these findings matter?
Adults using marijuana for pain reduction and/or recreational purposes should be aware of the dangers of opioids, and policymakers should weigh these risks when considering marijuana as a means to limit medical and nonmedical opioid use. Additionally, these findings exemplify the dangers of ecological fallacy. Population level data, such as the rates of statewide opioid-related deaths, should not be used to draw definitive conclusions about individuals.
Every study has limitations. What are the limitations in this study?
The NESARC did not distinguish between recreational and medical marijuana use; motivation for marijuana use could modulate the relationship between marijuana and prescription opioids. Data were collected from 2001 to 2005, and attitudes toward and usage patterns of marijuana may have since changed. Self-reporting of sensitive drug use information may underestimate prevalence.
For more information:
Our Addiction Resources page has free, anonymous resources for people concerned about substance use or other expressions of addiction.
— Jamie Juviler
What do you think? Please use the comment link below to provide feedback on this article.
________________
[1] “Nonmedical” is defined as using without a prescription, in greater amounts than prescribed, or for a reason other than prescribed.
[2] The researchers also adjusted for covariates including anxiety and mood disorders, and family history of drug, alcohol, and mental health problems.




Ken C. Winters, Ph.D. October 2, 2018
Thank you for highlighting this important article. My 2-cents: Olfson study is based on a prospective sample, an important design feature that is in contrast to prior correlational studies which suggested medical marijuana states are experiencing less opioid abuse problems (e.g., Bachbuber et al., 2014). It is way too early to claim that legalizing medical marijuana will make a dent in our opioid crisis.
Interested readers may also find this study from Australia of value (similar results as the Olfson study):
Campbell, G., Hall, W. D., Peacock, A., Lintzeris, N., Bruno, R., Larance, B., … & Blyth, F. (2018). Effect of cannabis use in people with chronic non-cancer pain prescribed opioids: findings from a 4-year prospective cohort study. The Lancet Public Health, 3(7), e341-e350.
James Juviler October 2, 2018
Hi Dr. Winters,
Thank you for your comment, and for mentioning the power of prospective data. Studies like Bachbuber et al., 2014 are interesting, but can easily be interpreted by the general public as promoting marijuana as a “miracle cure”, especially when reported by a secondary source. We hope our reviews promote scientific literacy and prevent such misunderstanding.
Best,
James Juviler
Jennifer Smith December 30, 2018
Cannabis is a great pain reliever. I use it for my migraine attacks. It’s all worth it!
Kevin Murphy July 28, 2019
Opioid use and cannabis use are two different matters. But of course, opioids provide higher side effects but you should also be careful depending on cannabis too much. Nice research!