Editor’s Note: We’re proud to announce that Dr. Daniel Alford will speak on the topic of “Best Practices in Treating Opioid Use Disorders with Medications” at this fall’s Addiction Medicine continuing medical education course, presented by the Division on Addiction through Harvard Medical School. In today’s article, we review research from Dr. Alford and his colleagues at the Clinical Addiction Research and Education (CARE) Unit at the Boston University School of Medicine.
People who struggle with chronic pain often experience daily difficulties, such as depression and anxiety symptoms, sleep disturbance, substance use, and increased use of healthcare systems. Because chronic pain is difficult to treat, patients might seek relief outside of typical medical pathways. This week, STASH reviews a study by Daniel Alford and his colleagues that looks at the prevalence of primary care patients with chronic pain and pain related dysfunction, as well as a history of self-medication with substances.
What is the research question?
How many primary care patients with recent drug use have chronic pain and use substances to manage it?
What did the researchers do?
Alford and his colleagues enrolled 589 primary care patients with at least one self-reported instance of illicit drug use or prescription drug misuse in the past 3 months. The researchers asked patients about their chronic pain, pain-related dysfunction, substances used to treat pain, mental health, and demographic information.
What did they find?
About 84% of patients reported having any kind of chronic pain, and 74% of patients reported having pain-related dysfunction. In all, 51% of patients who reported using marijuana, cocaine, or heroin during the last 3 months reported that they did so in order to treat their pain. Furthermore, 81% of patients who misused prescription medication, and 38% of patients who heavily used alcohol, stated that they did so to treat their pain (Figure 1).
Why do these findings matter?
Substance misuse for chronic pain is a serious public health concern. Some people who have chronic pain might become dependent on opioids or other substances, prescribed or not. The recent coverage of the opioid epidemic has shed some light on how prescribing opioids can be potentially harmful to some patients, but one study shows that treating drug dependence alone is not enough when chronic pain is still an underlying issue. The misuse/abuse of these substances can lead to fatal drug overdoses and other dangerous health problems.
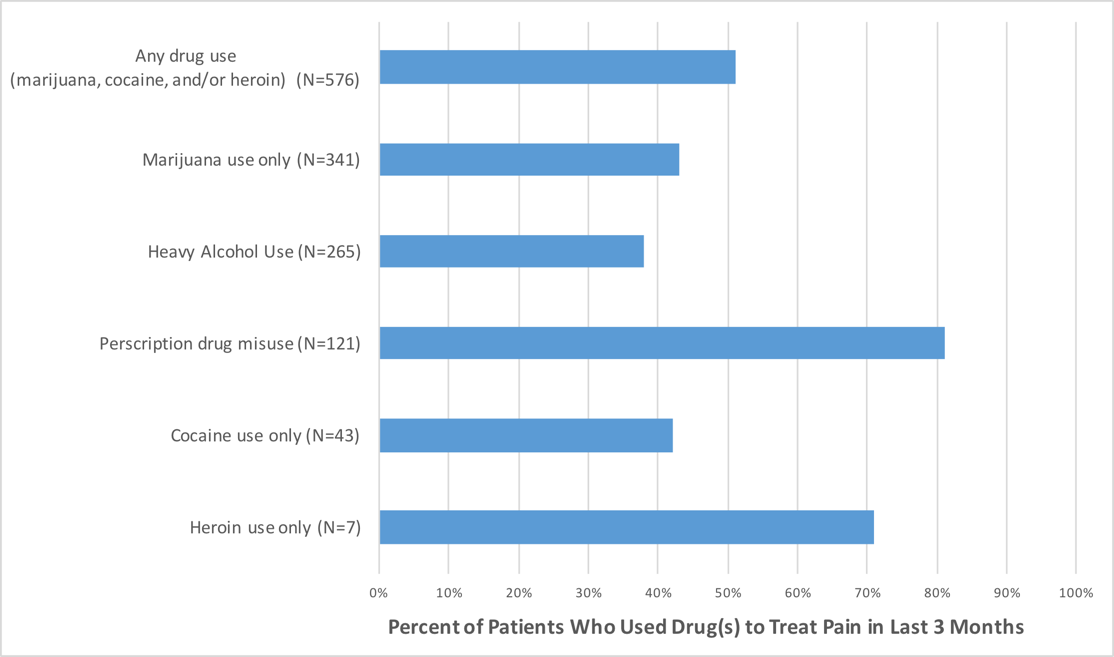
Figure. A large number of patients reported using substance to treat pain. All individual substance groups are mutually exclusive. Figure created from Alford et al., 2016. Click image to enlarge.
Every study has limitations. What about this one?
The results are all based on self-reported statements, which could be wrong. Additionally, this study does not show that chronic pain caused substance use, though a majority of patients reported that this was their experience. A longitudinal study—a study that follows the same people over time—could help us understand and combat the misuse of substances to treat chronic pain.
For more information:
If you or a loved one has a problem with substance use, please visit our addiction resources here.
For help with finding substance use treatment please click here to visit the Substance Abuse and Mental Health Services (SAMHSA) webpage.
SAMHSA also has a 24/7 hotline you can reach at this number: 1-800-662-HELP (4357)
— Alec Conte
What do you think? Please use the comment link below to provide feedback on this article.




-E.N. August 10, 2016
My husband is in chronic pain. He does not drink and has never abused drugs. He does not sleep, no longer goes anywhere but to doctors appointments. He is treated by caregivers as “an addict”. His pain is dismissed. My husband is bent over now and can only walk a few steps. He has daily migraines, kidney stones and has numerous health problems. He is given an injection in his hip 3 or 4 times a year which helps some.
I am home with him so I know he does not sleep or go out. His last back surgery put titanium in his back. All I know is that after the surgery when he was briefly on pain medication he could stand straight. I would love him to have narcotics so that he can have a life and function. He uses EFT to help and has a d.a.v.i.d. Device that moderates brain waves to a more relaxed state. The medical field has failed him. I read about how mindfulness helps but no one has offered that. I read about surgery to insert a machine to help with pain polyvagal stimulation? I believe the wealthy get help and the impoverished are kept suffering.