Did you know that methadone maintenance treatment (MMT), is one of the most effective treatments for opioid use disorders, especially when patients stay in treatment for at least 12 months? In fact, stopping MMT prematurely risks negative outcomes, including death. As a result, a group of researchers recently studied which patients are most at risk for stopping MMT too soon. Today, as part of our Special Series on Opioid Dependence and Recovery, we review their study.
What is the research question?
Which factors predict stopping methadone maintenance treatment too early?
What did the researchers do?
Steven Proctor and his colleagues gathered patient record data from a large substance use treatment program in the United States. They used data from 1,644 MMT patients. The modal patient was male, between 18-74 years old, White, and unemployed. The researchers used logistic regression to determine what characteristics predicted being discharged from treatment before 6 months and before 12 months. The most common reason for discharge was leaving against medical advice.
What did they find?
Almost 50% of the patients were still in treatment 6 months after starting, and about 20% were still in treatment at 12 months. Some predictors warned of discharge just a few months after starting treatment. Specifically, being Hispanic, unemployed, and single, and using cocaine at intake all increased the risk for being discharged before 6 months. Other predictors warned of discharge later, but still prematurely. Male gender, being younger than 35, paying for treatment out-of-pocket, cocaine use at intake, and opioid use at 6 months all predicted discharge before the 12 months. In fact, patients who used cocaine at intake were nearly 4 times more likely to be discharged at 12 months (see Figure 1). Being on a relatively low dose of methadone also increased the risk for premature discharge.
Why do these findings matter?
Opioid dependence is complex and influenced by many factors, so treatment should not be one-size-fits-all. Armed with these results, treatment providers can devote specialized resources to patients who are most at risk for early discharge from MMT. For example, providers could connect unemployed patients with job skills programs, so they will have fewer barriers to staying in treatment for the long term. Similarly, patients from ethnic minority groups might benefit from culturally adapted treatments, unmarried patients might benefit from programs that strengthen their social networks, and patients using cocaine might benefit from psychosocial approaches (e.g., cognitive-behavioral therapy, contingency management) embedded within their MMT.
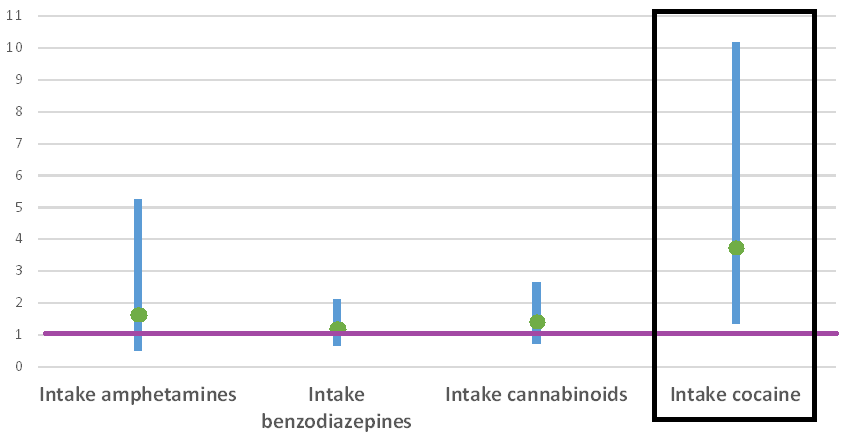
Figure. Substance use predictors showing increased risk of being discharged from MMT before 12 months. The green circles represent odds ratios and the blue lines represent 95% confidence intervals. Odds ratios greater than 1 indicate increased risk for premature discharge. The effect is only statistically significant for cocaine use at intake. Click image to enlarge.
Every study has limitations. What about this one?
Although the researchers have found that certain behaviors, like using cocaine at the start of MMT, predict increased risk for premature discharge, they cannot be certain that these behaviors cause increased risk. For example, using cocaine at intake could be a proxy for other characteristics that cause premature discharge. Still, these indicators help pinpoint patients who might need additional support to stay in treatment.
For more information:
The National Institute on Drug Abuse provides more information about methadone maintenance therapy and other treatments for opioid dependence here. You can find U.S. providers who treat substance use disorders here.
— Heather Gray
What do you think? Please use the comment link below to provide feedback on this article.




David Wilson June 15, 2016
I’ve provided outpatient opiate addiction treatment for more than 30 years. A substantial portion of those I’ve seen who left methadone treatment prematurely were terminated involuntarily by the programs for usage of other drugs or missed doses.
The statistics shown do not reflect this type of premature termination. I think that such terminations deserve special attention and should be reflected in the statistics.
Alan Wartenberg MD, FACP, DFASAM June 15, 2016
This information is not new, and corroborates studies dating back into the early 1970s, including a very good study in JAMA by Karen Sees from San Francisco over 10 years back, which showed that 2 years appeared to be the dividing point. However, as long as we have an ideology in 12 step treatment advocates that equates maintenance treatment with continued use of street drugs, we will never get the support, and will never rid ourselves of the stigma connected not only with methadone, but with buprenorphine treatment. 12 step treatment is very successful for a subset of patients, but people within this subset, seeing only each other, do not understand what a selection bias means, and think that everybody can do what they did, and they are just not trying hard enough. Elsewhere, this would be called blaming the victim. However, in 12 step circles, the trick is to blame “money hungry legalized drug pushers” (like me and thousands of my colleagues), not allow people on MAT to speak at meetings, not consider them “clean or sober,” pressure them to discontinue their treatment, and other indignities. It also allows these same people to violate 12 step traditions and take political action in restricting funding for MAT as well as influencing legislators, regulators and the general public into restricting adequate funding for programs that can help far more people than does 12 step treatment.