Military service members and veterans are more likely to smoke than members of the general population (McKinney et al., 1997). Researchers have been investigating both the reasons for the increased rates of nicotine use and any factors that might give military personnel who smoke better chances of successfully quitting. This week, as part of our Special Series on Addiction among Military Personnel and Veterans, the ASHES reviews a prospective study that explored both smoking initiation and quitting among soldiers deployed to Iraq (Harte et al., 2014).
Methods
- A total of 773 active duty and activated National Guard soldiers from the Neurocognition Deployment Health Study (Vasterling et al., 2006) participated.
- Participants completed their Time 1: before deployment assessment between April 2003 and July 2004. They completed their Time 2: after deployment assessment between January 2005 and September 2006.
- At both assessments, participants were asked the average number of cigarettes smoked per day and the amount of alcohol consumed in a typical week.
- Additionally, at both times researchers measured the participants’ perceived military unit cohesion (e.g., social bonds, loyalty, trust), and the severity of any PTSD symptoms.
- At Time 2, the researchers measured participants’ perceived exposure to traditional combat and non-combat stressors (e.g., handling bodies, seeing the bodies of dead civilians).
- The researchers used logistic regression on those who were not smokers at Time 1 to test which variables were predictors of smoking initiation at Time 2. Similarly, using participants who were smokers at Time 1, they tested which variables were predictors for smoking cessation use at Time 2.1
Results
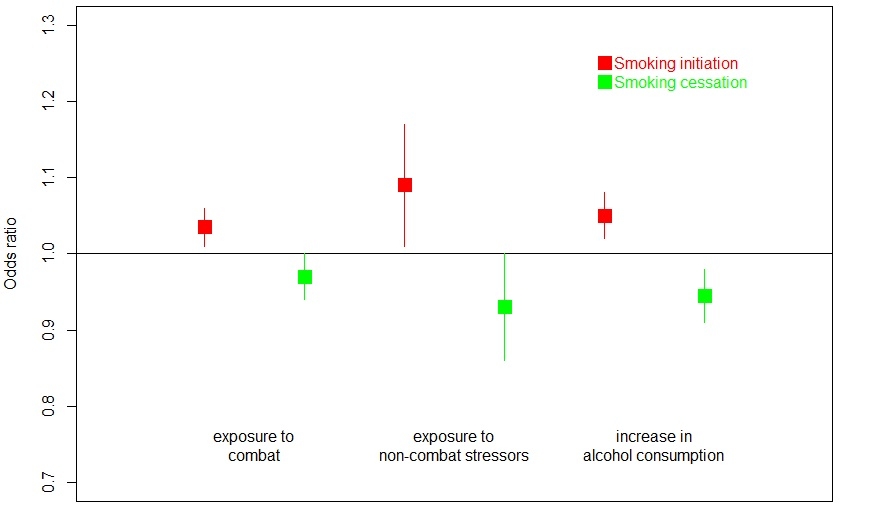
- Among the deployed personnel who did not smoke at Time 1, those who later started smoking reported higher traditional combat exposure (odds ratio [OR] = 1.03, 95% Confidence Interval [1.01,1.06]), higher exposure to non-combat stressors (OR = 1.09, 95% CI [1.01,1.17]), and a greater increase in alcohol consumption from Time 1 to Time 2 (OR = 1.05, 95% CI [1.02,1.08]) than those who did not start smoking.
- Among the deployed personnel who smoked at Time 1, those who later quit smoking reported lower exposure to non-combat stressor (OR = 0.93, 95% CI [0.86,1.00]) and a smaller increase in alcohol consumption from Time 1 to Time 2 (OR = 0.95, 95% CI [0.91,0.98]) than those who did not quit smoking.
- PTSD and changes in PTSD symptoms were not significant predictors in either model.
Figure. Unadjusted odds ratios (boxes) and 95% confidence intervals (lines) for combat stress levels, non-combat stress levels, and increases in alcohol consumption levels. Odds ratios above 1.0 with confidence intervals that do not include 1.0 represent increased risk for smoking initiation relative to those with lower combat or non-combat exposure or less of an increase in alcohol consumption. Odds ratios below 1.0 with confidence intervals that do not include 1.0 represent an increase in chance of quitting smoking relative to those with higher exposure to non-combat stressors or greater increases in alcohol consumption. Adapted from Harte et al. (2014). Click image to enlarge.
Limitations
- The sample was U.S. Army personnel. It may not be representative of all U.S. armed forces personnel as a whole.
- Women and commissioned officers were underrepresented in the sample.
- Most of the data, including the smoking and alcohol consumption rates, were self-reported. Participants’ answers might have been biased by their memory or by their personal attitudes about smoking and drinking.
Conclusion
It should come as no surprise that exposure to stressful combat and non-combat events is positively associated with initiating smoking and negatively associated with quitting. There have been many news articles and features reporting the links between the stress soldiers experience in war and the mental health problems they suffer later on in life. While larger looming problems such as PTSD have had more of the spotlight (and deservedly so), nicotine use also poses a significant threat to veterans’ health. Providing veterans with comprehensive, accessible, and integrated medical and mental health services might reduce the rates of post-deployment smoking and other expressions of addiction, thereby producing long-term improvements in quality of life.
Are you, or is a loved one, a U.S. service member who wants help to quit smoking? Check out these resources sponsored by the U.S. Department of Defense. For additional tools, please visit the BASIS Addiction Resources page.
— Matthew Tom
References
Harte, C. B., Proctor, S. P., & Vasterling, J. J. (2014). Prospective examination of cigarette smoking among Iraq-deployed and nondeployed soldiers: Prevalence and Predictive Characteristics. Annals of Behavioral Medicine. doi:10.1007/s12160-013-9584-5
McKinney, W. P., McIntire, D. D., Carmody, T. J., & Joseph, A. (1997). Comparing the smoking behavior of veterans and nonveterans. Public Health Reports (Washington, D.C.: 1974), 112(3), 212–217; discussion 218.
Vasterling, J. J., Proctor, S. P., Amoroso, P., Kane, R., Gackstetter, G., Ryan, M. A. K., & Friedman, M. J. (2006). The Neurocognition Deployment Health Study: A prospective cohort study of Army Soldiers. Military Medicine, 171(3), 253–260.
What do you think? Please use the comment link below to provide feedback on this article.
________________
1 Both logistic regressions included Time 1 PTSD Checklist score, change in the checklist score between Time 1 and Time 2, reported weekly alcohol consumption at Time 1, and change in weekly alcohol consumption between Time 1 and Time 2 as predictors.