Like most addictive behaviors, relapse is common among individuals who attempt to quit smoking (Shaffer et al., 2004). However, the identification of markers for high risk of smoking relapse could facilitate lasting, or longer, periods of smoking cessation by creating opportunities to intervene (e.g., improve treatment, emphasize relapse prevention). This week, ASHES reviews a recent study, which examined whether pre-cessation reactivity to smoking-related images and words could mark increased risk for smoking relapse (Janes et al., 2010).
Methods
- 21 women who met DSM-IV criteria for current nicotine dependence, smoked at least 10 cigarettes per day during the previous 6 months, expired more than 10 ppmv air CO, and were scheduled to participate immediately in an 8-week smoking cessation clinical triali, participated in this study.ii
- Participants completed a variety of paper-pencil survey items, as well as two smoking cue reactivity tasks: (1) a Stroop task (i.e., researchers used a computer program to record the accuracy and time required for participants to report the word color for smoking-related and neutral words); and (2) cue-related neuroimaging (i.e., participants viewed smoking-related, neutral, or animal images during fMRI scans).
- Participants reported smoking behavior each week using the Timeline Followback Method and expired CO measurement.
- The researchers operationally defined individuals who quit smoking for 24 hours as abstinent if their study-wide weekly smoking report included CO<9 ppmv and no self-reported smoking; they considered all others (n=9) as “slipped.”
Results
Compared to individuals who did not slip, those who reported that they had slipped showed more baseline fMRI reactivity to smoking cues in multiple brain areas, t(19)=2.86, cluster corrected, p<.01,iii and baseline smoking-related Stroop effects for accuracy, F(1, 16)=7.98, p<.05, and timing, F(1, 16)=7.30, p<.05, of responses, after controlling for assessed nicotine dependence (see Figure).
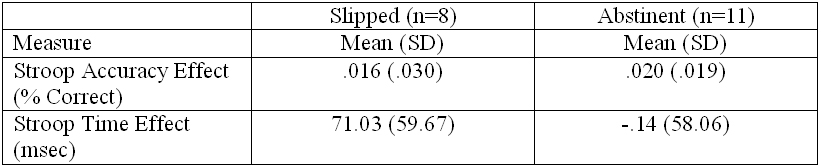
Figure. Baseline mean and standard deviations by post-quit smoking group. Click image to enlarge.
Note. Only 8 of 9 individuals who “slipped” completed the Stroop task.
Limitations
- The study included only a small number of women seeking help for quitting smoking, which might affect generalizability of these results.
- The study took place within a co-occurring smoking cessation trial; therefore, the participants are help-seekers, who might be different from smokers more generally. This circumstance also can limit the generalizability of these findings.
Discussion
The identification of objective markers of risk for addiction-related relapse behavior is important. Identifying markers can help guide treatment planning and matching, and smoking prevention efforts. This study represents a preliminary step toward the development of an early warning system for smoking relapse risk. Relapse cue training could become an important treatment component for providers and help-seekers. Additional research should include practical considerations of the use of fMRI in risk assessment, a determination of the durability of such predictive markers over time, and the identification of other possible behavioral markers of risk for relapse.
References
Janes, A. C. et al., (2010 online first). Brain reactivity to smoking cues prior to smoking cessation predicts ability to maintain tobacco abstinence. Biological Psychiatry.
Shaffer, H. J. et al., (2004). Toward a syndrome model of addiction: Multiple expressions, common etiology. Harvard Review of Psychiatry, 12(6), 367-374.
What do you think? Please use the comment link below to provide feedback on this article.
________________
i During the 8 week study each participant received individual behavioral intervention, the patch, and nicotine gum or lozenges as needed.
ii Exclusions included: unstable medical illness; pregnancy; recent drug and alcohol use; major depressive disorder; alcohol use disorder in prior 6 months; current psychotropic drug use; or lifetime diagnosis of organic mental or psychotic disorders.
iii Elevated reactivity occurred for the bilateral insula, ACC, posterior cingulated cortex, inferior parietal cortex, paraphippocampal gyrus, thalamus, putamen, cerebellar hemispheres and vermis, prefrontal cortex, and striate and extrastriate corex.