Gambling harm is a significant issue among culturally and linguistically diverse (CALD) community members who live in disadvantaged areas in Australia. This problem is exacerbated by the fact that gambling harm assessment options require gamblers to self-disclose to healthcare providers, as CALD community members are less likely to discuss gambling with their providers due to stigma and language barriers. One potential solution is to implement screening for gambling-related problems in primary and community care settings, which could help improve access to Gambling Disorder treatment for CALD community members. This week, The WAGER reviews a study by Andrew Reid and colleagues that examined enablers of and barriers to a pilot study that implemented a gambling harm screening model in primary and community care settings.
What was the research question?
What are some enablers of and barriers to implementing a gambling harm screening model for CALD community members in primary and community care settings?
What did the researchers do?
The researchers implemented a problem gambling screening and referral model in general practice and community-based services in Fairfield, Australia, an area with a large CALD population. The screening model included the Problem Gambling Severity Index short form and the Concerned Others Gambling Screen. If the client screened positive for being at-risk for gambling harm on either measure, the provider would give them a list of gambling help resources for them to read and contact.
Following implementation, the researchers conducted interviews with two general practitioners and seven community workers who administered the screening model with 130 patients. The goal was to learn about factors that facilitated and hindered the implementation of the screening model.
What did they find?
One structural factor that facilitated implementation was alignment with standard consultation procedures (see Figure for key enablers and barriers). Participants indicated that it was easy to integrate the screening model, as it supported their existing holistic patient care approaches. Process-related factors that facilitated implementation included the screening assessment’s online format and short length, which made it easier to administer and increased its accessibility to patients. One social factor that facilitated implementation was increased staff knowledge and empowerment. Participants explained that taking part in the pilot project increased their confidence in discussing gambling with patients and addressing gambling harm.
One structural factor that hindered implementation was a lack of long-term funding, which created uncertainty about the continued development and expansion of gambling interventions (see Figure). One process-related factor that hindered implementation was an unclear referral model. The model only provided patients with a list of resources for them to contact themselves, so providers were not able to adequately support their patients through this process. Finally, a social factor that hindered implementation was the complexity of gambling harm, as some patients seemed to be in greater need of other services, such as mental health and financial services, compared to gambling help services.
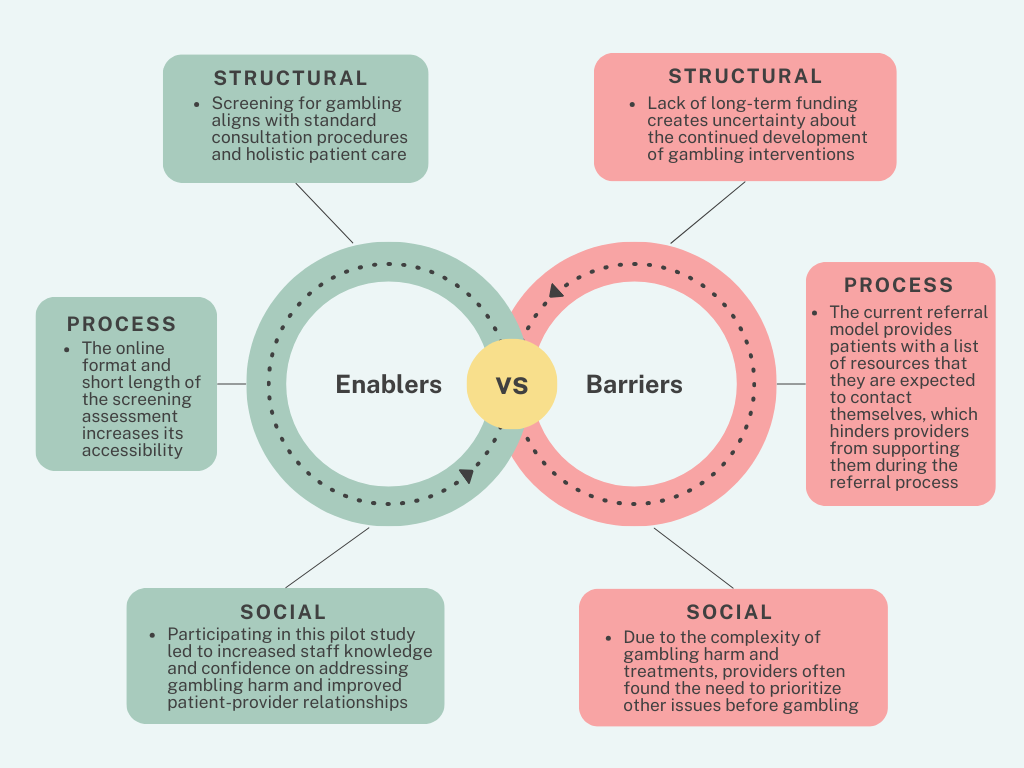
Figure. An overview of key enablers and barriers to the implementation of the gambling harm screening and referral model. Click image to enlarge.
Why do these findings matter?
Integrating problem gambling screening in primary healthcare and community service settings can help to support holistic patient care procedures, increase access to gambling support services, and mitigate gambling harm within communities. Primary care providers who are involved in discussing gambling with their patients can also play a role in reducing stigma related to gambling issues and help-seeking by using person-first, humanizing language. The current study highlights the importance of not only increasing access to gambling harm screening, but also providing support and referring patients to appropriate gambling help resources.
Every study has limitations. What are the limitations in this study?
One limitation is that the researchers only interviewed nine participants who were general practitioners and community workers; they did not interview other people such as practice nurses and practice owners who were also involved in implementing the screening model. Additionally, to better evaluate the effectiveness of the problem gambling screening model, future research should examine the model’s acceptability from the perspective of community members from different cultural backgrounds.
For more information:
Individuals who are concerned about their gambling behaviors or who simply want to know more about problem gambling may benefit from visiting the National Council on Problem Gambling or Gamblers Anonymous. Additional resources can be found at the BASIS Addiction Resources page.
— Annette Siu
What do you think? Please use the comment link below to provide feedback on this article.




