Rates of tobacco use are disproportionately high among individuals with substance use disorders (SUD), including those in addiction treatment. California has taken measures to prioritize tobacco cessation among these individuals. The state’s Tobacco-Free for Recovery Initiative supports residential SUD treatment programs in implementing tobacco-free grounds policies (i.e., no tobacco use by clients or staff on program grounds) and other measures that promote tobacco cessation. This week, ASHES reviews a study by Caravella McCuistian and colleagues that examined changes in smoking prevalence, tobacco use behaviors, and receipt of tobacco-related services by clients of residential SUD treatment programs participating in California’s Tobacco-Free for Recovery Initiative.
What was the research question?
Were there differences in smoking prevalence, tobacco use behaviors, and receipt of tobacco-related services among clients of residential SUD treatment programs before, during, and after program participation in the Tobacco-Free for Recovery Initiative?
What did the researchers do?
Seven residential SUD treatment programs received financial support and expert guidance to design and implement tobacco-free policies through the Tobacco-Free for Recovery Initiative. Clients currently enrolled in these programs completed surveys at three timepoints over 15 months: at the start of the intervention (i.e., baseline), at an interim timepoint, and at the end of the intervention (i.e., post-intervention). Participants at these timepoints represented independent, cross-sectional samples.
All participants reported current cigarette use and whether they had been screened for smoking status by a staff member. Current smokers reported tobacco use behaviors. Both current smokers and those who quit during treatment reported receipt of tobacco-related services: nicotine replacement therapy (NRT) or other pharmacotherapy, referral to a smoking cessation specialist or helpline, counseling, and whether quitting smoking was part of their treatment plan. The researchers assessed changes in smoking prevalence, tobacco use behaviors, and receipt of tobacco-related services across the three timepoints. They then assessed changes over time between the baseline and interim, and baseline and post-intervention timepoints.
What did they find?
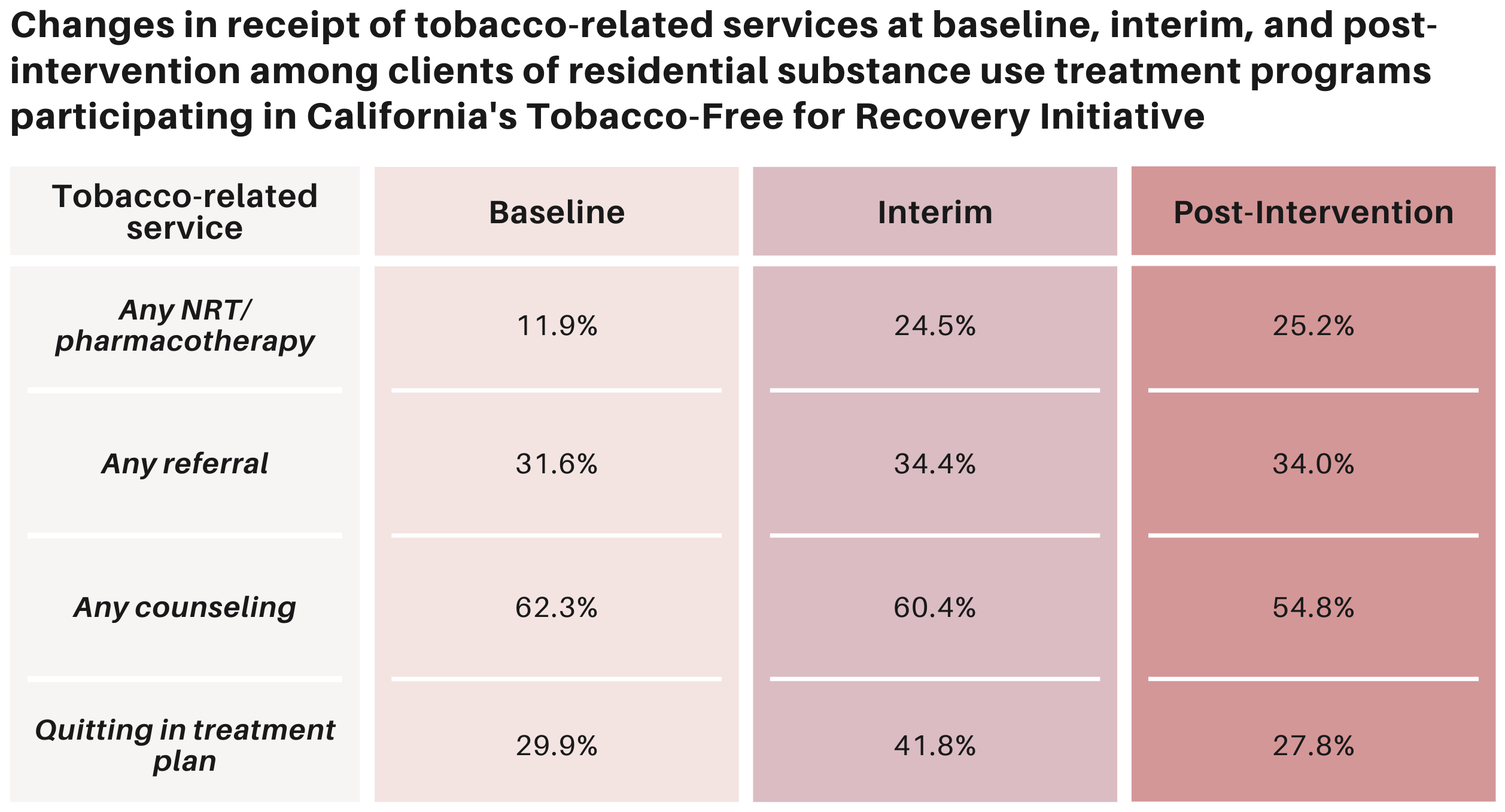
Five of the seven programs implemented tobacco-free policies. At these sites, client smoking prevalence decreased from 54.2% at baseline to 26.6% at post-intervention. More than half of participants (60.2%) reported being screened for smoking at baseline and this remained relatively unchanged at post-intervention. Current smokers and those who quit during treatment reported an increase in NRT/pharmacotherapy from baseline (11.9%) to post-intervention (25.2%). Receipt of referrals and quitting smoking as part of the client’s treatment plan remained relatively unchanged from baseline to post-intervention, while tobacco-related counseling decreased (see Figure). Clients were less likely to report being a current smoker at post-intervention compared to baseline. Current smokers and those who quit while in treatment were more likely to receive NRT/pharmacotherapy at post-intervention compared to baseline.
Figure. Changes in receipt of tobacco-related services at three timepoints (baseline, interim, and post-intervention) among clients of residential SUD programs participating in the Tobacco-Free for Recovery Initiative. Adapted from McCuistian et al. (2022). Click image to enlarge.
Why do these findings matter?
This study found that interventions that support residential SUD treatment programs in implementing tobacco-free grounds policies might lead to a decrease in prevalence of client smoking and increase in the receipt of NRT and pharmacotherapy. Increased efforts should be made to support residential SUD programs in implementing tobacco-free policies, such as mandating SUD treatment programs assess and offer to treat tobacco use, or increasing staff training regarding the provision of tobacco-related services.
Every study has limitations. What are the limitations of this study?
This study used an observational, cross-sectional study design; as such, causality cannot be determined. In other words, we can’t say with certainty that the reduced prevalence of smoking or increase in NRT/pharmacotherapy were a result of this initiative. Findings may not be generalizable to non-residential SUD treatment programs or to programs found in other states or countries.
For more information:
SmokeFree offers tools and tips for quitting and maintaining abstinence from smoking tobacco. The Centers for Disease Control and Prevention also provides research and tips about cigarettes and how to quit. For additional self-help tools, please visit the BASIS Addiction Resources page.
— Kira Landauer, MPH
What do you think? Please use the comment link below to provide feedback on this article.