Langenbucher, Bavly, Labouvie, Sanjuan, and Martin (2001) suggest that evidence about the psychological and behavioral predictors of pathological (level 3) gambling remain limited due to a diminutive and methodologically weak body of literature on the subject. As such, they studied a variety of predictors of pathological gambling using a sample drawn from eight substance use disorder (SUD) treatment centers in five Northeastern states.
The gambling behavior of research participants (N=372) was measured using the South Oaks Gambling Screen (SOGS; Lesieur & Blume). Thirteen percent of the substance abuse treatment-seeking sample (n=49) met criteria for pathological gambling. Variables relating to premorbid risk, current substance use patterns, and psychiatric comorbidity were examined as predictors of pathological gambling disorders.
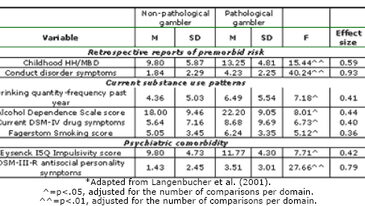
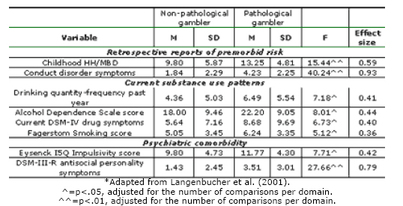
Langenbucher et al. (2001) point out that adolescent Hyperkinesis/Minimal Brain Damage–as indicated by the Hyperkinesis/Minimal Brain Damage (HK/MBD) Questionnaire (Alterman & McLellan, 1986)–and conduct disorder symptoms–as indicated by the Structured Clinical Interview for DSM-III-R (SCID; Spitzer, Williams, Gibbon, & First, 1988)–are correlated with the onset of pathological gambling and substance use disorders. Additionally, according to the Composite International Diagnostic Interview-Expanded Substance Abuse Module (CIDI-SAM; Robins, Cottler, & Babor, 1990), pathological gamblers are more dependent on alcohol than non-pathological gamblers. In addition, pathological gamblers drink in larger quantities and more frequently than those with less severe gambling disorders (Langenbucher et al., 2001).
Finally, impulsivity-measured by Eysenck Impulsivity Questionnaire (Eysenck, Pearson, Easting, & Allsopp, 1985)–and antisocial tendencies-measured by the SCID II–were predictors of pathological gambling (Langenbucher et al., 2001). These results, according to Langenbucher et al. (2001), relate to the presence of HK/MBD in childhood since these disorders sometimes evolve into impulsivity and antisociality during adulthood. Table 1 presents these and other significant predictors of pathological gambling.
Table 1. Psychopathological predictors of pathological gambling among an SUD cohort*
Data collected by Langenbucher et al. (2001) indicate that pathological gambling disorders are comorbid with SUDs. However, these results do not readily generalize to women and minorities since these population segments are not adequately represented in this study’s broad but demographically limited research sample. Nonetheless, this brief report (2001) shows that substance abuse treatment facilities and their providers need to screen for pathological gambling disorders since problems with gambling might affect SUD treatment strategies and the consequent efficacy of these treatments.
References
Alterman, A. I., & McLellan, A. T. (1986). A factor-analytic study of Tarter’s "Hyperactivity-MBD" Questionnaire. Addictive Behaviors, 11, 287-294.
Eysenck, S. B. G., Pearson, P. R., Easting, G., & Allsopp, J. F. (1985). Age norms for impulsiveness, venturesomeness and empathy in adults. Personality and Individual Differences, 6, 613-619.
Langenbucher, J., Bavly, L., Labouvie, E., Sanjuan, P. M., & Martin, C. S. (2001). Clinical features of pathological gambling in an addictions treatment cohort. Psychology of Addictive Behaviors, 15(1), 77-79.
Lesieur, H. R., & Blume, S. B. (1987). The South Oaks Gambling Screen (SOGS): a new instrument for the identification of pathological gamblers. American Journal of Psychiatry, 144, 1184-1188.
Robins, L. N., Cottler, L. B., & Babor, T. (1990). Composite International Diagnostic Interview–Expanded Substance Abuse Module (CIDI-SAM). St. Louis, MO: Author.
Spitzer, R. L., Williams, J. B. W., Gibbon, M., & First, M. (1988). Structured Clinical Interview for DSM-III-R–Patient Version. New York: Biometrics Research Department, New York State Psychiatric Institute.
The WAGER is a public education project of the Division on Addictions at Harvard Medical
School. It is funded, in part, by the National Center for Responsible Gaming, the
Massachusetts Department of Public Health, the Addiction Technology Transfer Center of
New England, the Substance Abuse and Mental Health Services Administration, and the
Center for Substance Abuse Treatment.