Nicotine dependence is the most common substance use disorder among people with mental illness (Lesser, Boyd et al. 2000; Grant, Hasin et al. 2004). Mentally ill patients who use tobacco are not only at great risk for developing tobacco-related diseases, but tobacco dependence also can disrupt psychiatric treatment (Hurt, Offord et al. 1996) . Nevertheless, on average, psychiatrists offer advice about smoking cessation during only 12% of patient visits (Himelhoch and Daumit 2003). This week’s ASHES reviews a national study that surveyed directors of psychiatry residency programs in the United States about nicotine dependence training in their programs.
Prochaska, Fromont, Louie, Jacobs, and Hall (2006) mailed questionnaires to the training directors of psychiatry residency programs identified on the American Medical Association’s Fellowship and Residency Electronic Interactive Database (N=181). These surveys included questions about the amount of time the programs devoted to tobacco dependence, perceptions of the residents’ skills in aiding patients with quit attempts, and interest in implementing a model tobacco treatment aspect to the curriculum. Approximately 63% of the targeted participants completed the surveys.
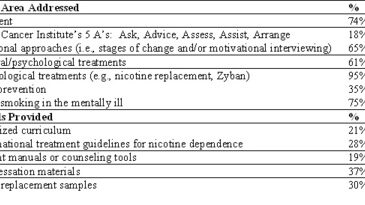
Results indicated that all of the programs included some form of addiction training, but only half of the programs specifically mentioned nicotine; further, only 43% of those that mentioned nicotine provided clinical experience with nicotine dependent psychiatric patients. Eighty-five percent of the programs including nicotine training only dedicated one hour to the subject, and 10.5% said their nicotine training program was optional. For more details about the content of the training programs see the Figure.
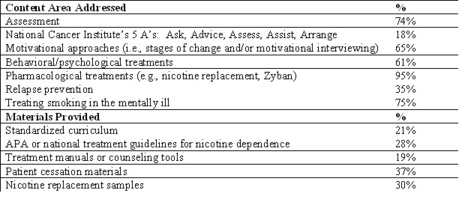
Figure. Prevalence of Content and Materials of Psychiatry Residency Programs with Tobacco Treatment Training (N=57) (Prochaska, Fromont et al, 2006). Click image to enlarge.
This study is not without limitations. Fewer than two-thirds of the targeted training programs responded. Consequently, there is potential for a response bias. The results also might not be representative of all training programs because of the large proportion of respondents from New York and California (23%). Despite these concerns, this research provides us with a map to the content of psychiatry program tobacco treatment training.
Hughes (1998) reported, “In terms of lives saved, quality of life, and cost efficacy, treating smoking is considered one of the most important activities a clinician can do.” Incorporating smoking cessation efforts into psychiatric treatment is strongly recommended (1996; Dalack and Glassman 1992) and therefore, psychiatry residency programs should expand their nicotine dependence treatment training. In addition, we encourage primary care and other training programs to integrate treatment training into their curriculum. Nicotine dependent patients enter the medical care system through various portals, and thus all health care providers need to be prepared for every opportunity.
References
(1996). “American Psychiatric Association: Practice guidelines for the treatment of patients with nicotine dependence.” American Journal of Psychiatry 153: 1-31.
Dalack, G. and A. Glassman (1992). “A clinical approach to help psychiatric patients with smoking cessation.” Psychiatry Quarterly 1992(63): 27-39.
Grant, B., D. Hasin, et al. (2004). “Nicotine dependence and psychiatric disorders in the United States: results from the national epidemiological survey on alcohol and related conditions.” Arch Gen Psychiatry 61: 1107-1115.
Himelhoch, S. and G. Daumit (2003). “To whom do psychiatrists offer smoking-cessation counseling?” American Journal of Psychiatry 160: 2228-2230.
Hurt, R., K. Offord, et al. (1996). “Mortality following inpatient addictions treatment: role of tobacco use in a community based cohort.” JAMA 275: 1097-1103.
Lesser, K., J. Boyd, et al. (2000). “Smoking and mental illness: a population based prevalence study ” JAMA 284: 2606-2610.
Prochaska, J. J., S. C. Fromont, et al. (2006). “Training in tobacco treatments in psychiatry: A national survey of psychiatry residency training directors ” Academic Psychiatry 30: 372-278.
What do you think? Please use the comment link below to provide feedback on this article.