Gambling-related problems often co-occur with other risky behavior patterns, such as excessive alcohol or substance use (Kessler et al., 2008). However, it is unclear whether efforts to address one behavior (e.g., gambling) will also lead to decreases in other problematic behaviors, or, instead, result in addiction-hopping, substituting one excessive behavior for another (Shaffer et al., 2004). This week, the WAGER reviews a study that examined the weekly alcohol use trajectories of treatment-seeking pathological gamblers to understand more fully the drinking patterns in that population (Rash et al., 2011).
Method
- Participants were 163 individuals taking part in one of two randomized clinical trials of psychotherapy for pathological gambling who reported any alcohol consumption in the 36-week period of data collection (56% of trial participants).
- Participants completed the timeline followback (TLFB) procedure at baseline, 8 weeks post-treatment, and 24 weeks post-treatment to report their alcohol use in the 12 weeks prior to gambling treatment, as well as the 24 weeks post-treatment.
- Based on the alcohol use data, researchers split participants into one of two groups:
- Ever-risky drinkers (n = 76) drank more than 14 standard drinks per week or four per day for males, and more than seven drinks per week or three per day for females on at least one occasion during the 12 weeks prior to treatment or 24 weeks post-treatment.
- Non-risky drinkers (n = 87) never drank at the above-specified risky levels during the course of the study.
Results
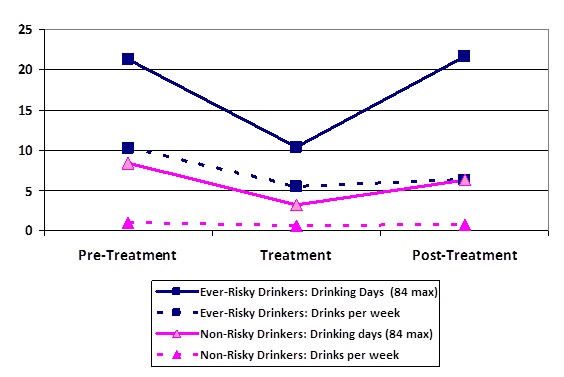
- Particularly among risky drinkers, alcohol use decreased prior to treatment entry, but then escalated again post-treatment.
- There were significant changes in at-risk status from the pretreatment period to the period following treatment entry. Fifty-five participants qualified as at-risk drinkers prior to treatment entry; 26 of those (47%) did not drink at risky levels after treatment entry. One hundred eight participants did not qualify as at-risk drinkers prior to treatment; however, 21 of those (19%) exhibited at-risk drinking after treatment entry.
Figure 1. Drinks per day and drinking days pre-, during, and post-gambling treatment (adapted from Rash et al., 2011).
Limitations
- The alcohol use data rely on retrospective self-report. Participants may have under- or over-estimated their alcohol use intake.
- Results are limited to gamblers-seeking treatment and do not provide information about whether the gambling treatment itself influenced alcohol-use patterns.
Conclusions
The reviewed study suggests that entry into gambling treatment might be associated with reductions in alcohol use. According to the syndrome model of addiction (Shaffer et al., 2004), various risky behavior patterns like excessive drinking or gambling may indicate an underlying addiction syndrome. However, the behaviors associated with that syndrome often follow different trajectories. Most risky gamblers who also drank reduced their drinking behavior post-treatment, but a small subset of the population persisted and actually worsened, suggesting that efforts to address one behavior may sometimes result in addiction-hopping.
– Kat Belkin
What do you think? Please use the comment link below to provide feedback on this article.
References
Kessler, R. C., Hwang, I., LaBrie, R., Petukhova, M., Sampson, N. A., Winters, K. C., & Shaffer, H. J. (2008). DSM–IV pathological gambling in the National Comorbidity Survey Replication. Psychological Medicine, 38, 1351–1360. doi:10.1017/S0033291708002900
Rash, C. J., Weinstock, J., & Petry, N. M. (2011). Drinking patterns of pathological gamblers before, during, and after gambling treatment. Psychology Of Addictive Behaviors, 25(4), 664-674.
Shaffer, H., LaPlante, D., LaBrie, R., Kidman, R., Donato, A., & Stanton, M. (2004) Toward a syndrome model of addiction: Multiple expressions, common etiology. Harvard Review of Psychiatry, 12(6), 367-374.