Research shows that the emergency room (ER) might be an important location for mental health screening and intervention, particularly drug and alcohol screening (Fleming et al., 2007). However, most ERs have limited time and resources to conduct such interventions. This week, the DRAM reviews a study examining the implementation and efficacy of an ER-based screening and brief intervention for young adults delivered through text messaging (Suffoletto, Callaway, Kristan, Kraemer, & Clark, 2011).
Method
- Participants were 45 individuals (41% of those initially recruited; 87% of those who screened in) recruited during emergency room visits. Participants were 18-24 years old and screened positive for hazardous drinking according to a past-three month version of the Alcohol Use Disorder Identification Test – Consumption (AUDIT-C: Dawson, Grant, & Stinson, 2005).
- At baseline and 12-week follow-up, all participants completed a computerized timeline follow-back (TLFB) assessment of their past-three month drinking, as well as the Rutgers Alcohol Problems Index to assess past-three month alcohol related problems.
- During the study, all participants received weekly texts for 12 weeks. Researchers randomized participants into one of three groups:
- Intervention (n = 15): Participants received weekly texts inquiring about their alcohol consumption. If they drank at hazardous levels during that week, they received additional texts asking them to set a goal to reduce their alcohol consumption during the next week and providing tips for reducing or assessing their drinking levels.
- Assessment (n = 15): Participants received the same text inquiry about their consumption as the intervention group, but no follow-up texts about reducing or assessing their drinking.
- Control (n = 15): Participants received weekly text messages reminding them that the researchers would ask them to complete a final survey at the end of the study.
Results
- Almost all (97%) of the young adult ER patients approached for the study willingly completed the AUDIT-C screen, and approximately half screened positive for hazardous drinking. All but one potential participant had access to a phone with text messaging capabilities. Retention was high: 70-80% of the participants in the assessment and intervention conditions responded to all 12 weekly texts, and more than 90% responded to at least one.
- According to weekly responses, participants who received the text-based intervention were less likely to have heavy drinking days (i.e., drinking more than 3 [women] of 4 [men] drinks in a single day) over the 12 weeks compared to participants in the assessment condition. Specifically, participants in the intervention condition had fewer weeks with a heavy drinking day (Median=2, IQR=1-7, compared to Median=7, IQR=3-9), and were less likely to have back-to-back weeks with heavy drinking days (58%, 95% CI=47-68, compared to 69%, 95% CI=58-79) than participants in the assessment condition.
- According to comparisons between the baseline and follow-up TLFB assessments of prior month drinking, participants in the intervention condition decreased their heavy drinking days and drinks per day, whereas participants in the assessment condition increased their heavy drinking days and drinks per day (see Figure).
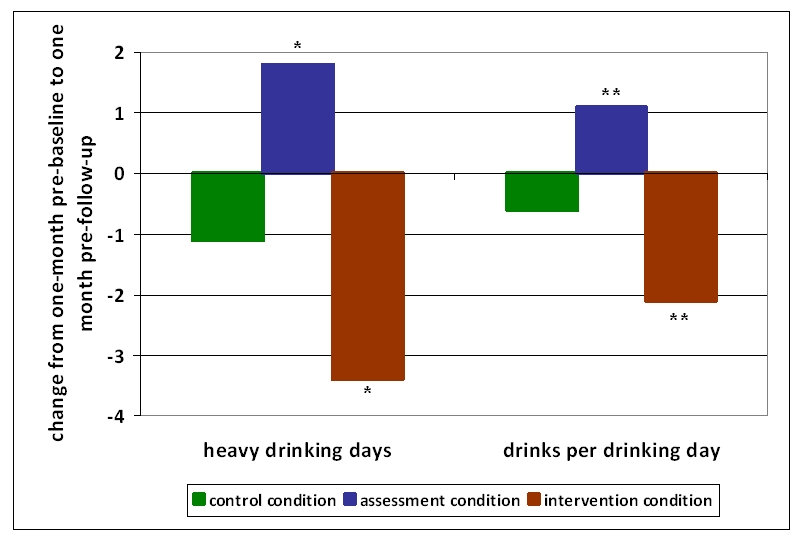
Figure. Change in drinks per day and heavy drinking days from baseline to 12-week follow-up (adapted from Suffoletto et al., 2011). Click image to enlarge.
*p<.05 between conditions for change in number of heavy drinking days; **p<.001 between conditions for change in number of drinks per drinking day
Note. Negative numbers represent decreases.
Limitations
- The small sample size and short follow-up period limit the strength of the study.
- Control participants’ 12-week follow-up data might have been less accurate than other participants’ follow-up data, because researchers did not prompt them to remember their alcohol consumption on a weekly basis.
Conclusions
Suffoletto et. al’s study suggests that text messaging might be a promising brief intervention strategy, particularly for young adults. As communication channels become more advanced and innovative, public health approaches should explore the value of utilizing contemporary channels for promoting positive health behavior.
-Sarah Nelson
What do you think? Please use the comment link below to provide feedback on this article.
References
Dawson, D. A., Grant, B. F., & Stinson, F. S. (2005). The AUDIT-C: screening for alcohol use disorders and risk drinking in the presence of other psychiatric disorders. Compr Psychiatry, 46(6), 405-416.
Fleming, E. A., Gmel, G., Bady, P., Yersin, B., Givel, J. C., Brown, D., et al. (2007). At-risk drinking and drug use among patients seeking care in an emergency department. J Stud Alcohol Drugs, 68(1), 28-35.
Suffoletto, B., Callaway, C., Kristan, J., Kraemer, K., & Clark, D. B. (2011). Text-Message-Based Drinking Assessments and Brief Interventions for Young Adults Discharged from the Emergency Department. Alcohol Clin Exp Res.