Today’s review is part of our month-long Special Series on Open Science Practices in addiction research. During this special series, The BASIS features recent publications that have used contemporary open science practices.
Recently, patient centered care (PCC) has been gaining momentum as a treatment strategy. Simply put, PCC aims to prioritize each patient’s unique needs by fostering patient-physician communication and shared decision making. This flexible method of care might be especially important in a complex disease such as addiction with its diverse array of expressions. However, different researchers have used different definitions of PCC and we know little about how it is understood within addiction treatment research and practice. This week, as part of our Special Series on open science, STASH reviews a preregistered article by Kristen Marchand and colleagues that described the defining features of existing research regarding PCC for addiction.
What was the research question?
In what ways have researchers examined, defined, and measured PCC core principles and outcomes as they relate to addiction care?
What did the researchers do?
The researchers collected studies relating to PCC from electronic databases and unpublished reports.1 They recorded how often each article described four defining characteristics of PCC (i.e., therapeutic alliance, shared decision-making, individualized care, and holistic care) and four outcome categories (i.e., substance use, treatment engagement, health and psychosocial outcomes and patient-reported experiences). In accordance with open science protocol, prior to conducting the study the researchers preregistered their protocol with the Open Science Framework and provided open access to the methodological details and dataset used in analysis.
What did they find?
The researchers collected 149 articles. They found that 72% of the articles described therapeutic alliance, defined as empathy and non-judgment. Less commonly, the articles described shared decision making (36%), individualized care (40%) and holistic care (24%) (see figure). Substance use was the most commonly measured outcome category (51%), followed by treatment engagement (49%), health and psychosocial outcomes (39%), and patient-reported experiences (18%).
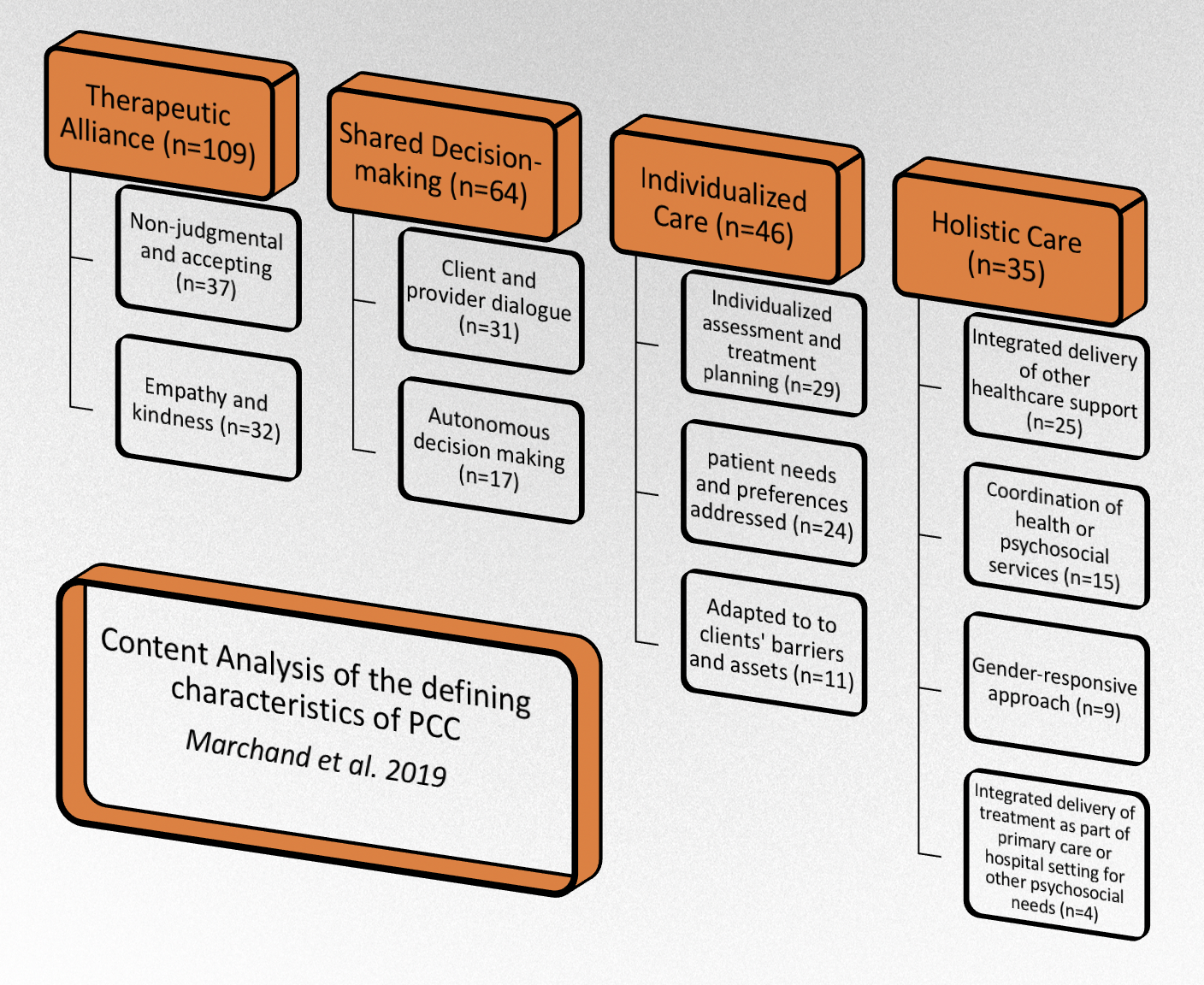
Figure. The most common principles of PCC for addiction included in the existing literature (in orange boxes) and their defining characteristics (in white boxes). The numbers in parentheses represent the number of articles in each of the categories, which are not mutually exclusive. The researchers did not assign defining characteristics to all of the articles. This explains why therapeutic alliance and shared decision-making have more articles than their respective defining characteristics combined. Click image to enlarge.
Why do these findings matter?
This was the first study to summarize how researchers in the field of addiction define PCC, which outcomes/principles they prioritized, and which areas need more work. For example, they only identified 4 studies that look at the integrated delivery of addiction treatment as part of a primary care or hospital setting for other health or psychosocial needs. It’s hard to justify mass implementation of such practices without further inquiry. So, this finding provides a strong rationale for researchers to devote increased time and resources to infrequently studied areas. At the same time, this paper informs healthcare providers and administrators which practices rest on a strong evidence base, and which might require additional research before they can be considered evidence-based practices.
Every study has limitations. What are the limitations in this study?
One limitation of this study (along with other scoping reviews) is that it is bound by its search and inclusion terms. Different search and inclusion terms might lead to a different list of articles examined, and therefore different conclusions and observations. Additionally, the researchers limited their search to articles written in English, French, Portuguese, Spanish and Italian, so research from North America and Europe was prioritized. Embracing research from other continents and cultures would likely boost representativeness.
For more information:
Are you worried that you or someone you know has an addiction? The SAMHSA National Helpline is a free treatment and information service available 24/7. For more details about addiction, visit our Addiction Resources page.
For an in depth background on patient-centered care you can visit: https://catalyst.nejm.org
— Alex LaRaja
What do you think? Please use the comment link below to provide feedback on this article.
________________
[1] Two independent reviewers screened the articles for their relevance. In order to be included in the final analysis articles needed to (1) include patients with substance related disorders (2) describe PCC (3) take place in a health care context for substance use disorder (4) be published between 1960 and July, 2018 (5) operationally define PCC approach (6) and quantitatively measure some form of patient outcome.