Healthcare providers working in emergency departments (ED) are positioned to identify victims of human trafficking and offer essential trauma-informed care. Many trafficked individuals who visit EDs likely need substance use disorder care, given that traffickers often use substances to recruit and control victims, and victims often use substances to cope with their trauma. This week, STASH reviews a study by Nathaniel A. Dell and colleagues that identified the prevalence of substance use disorders during ED visits in the US involving patients who have experienced human trafficking.
What was the research question?
Among ED patients who were suspected or confirmed to be victims of human trafficking, how commonly were substance use disorders diagnosed? Are substance use disorders equally common among sex trafficking victims and labor trafficking victims?
What did the researchers do?
The researchers examined data from the 2019 to 2021 Nationwide Emergency Department Sample, a record of visits to approximately 1,000 EDs across the US. Specifically, they examined the diagnostic codes that healthcare providers entered into patients’ charts. Their sample included 1,688 ED visits when providers documented that the patients were victims of human trafficking – either sex trafficking or labor trafficking. The researchers examined how often substance use disorders (SUDs) were diagnosed during these visits. They focused on SUDs other than nicotine use disorder.
What did they find?
Sex trafficking was coded in 78.9% of the human trafficking visits, and labor trafficking was coded in the remaining 21.1%. Overall, non-nicotine SUDs were documented in 37.6% of visits, most commonly stimulant use disorders (16.0%), followed by cannabis (14.9%), opioid (9.1%), alcohol (7.3%), and cocaine (7.7%) use disorders. Non-nicotine SUDs were more common among victims of sex trafficking, compared to labor trafficking (43.5% versus 15.8%). Sex trafficking victims, in particular, were more likely to experience cannabis use disorders, other substance use disorders, and non-nicotine polysubstance use disorders (see Figure). During visits when a patient was diagnosed with an SUD, the patient was more likely to be hospitalized (53.3%), compared to visits without an SUD diagnosis (12.4%).
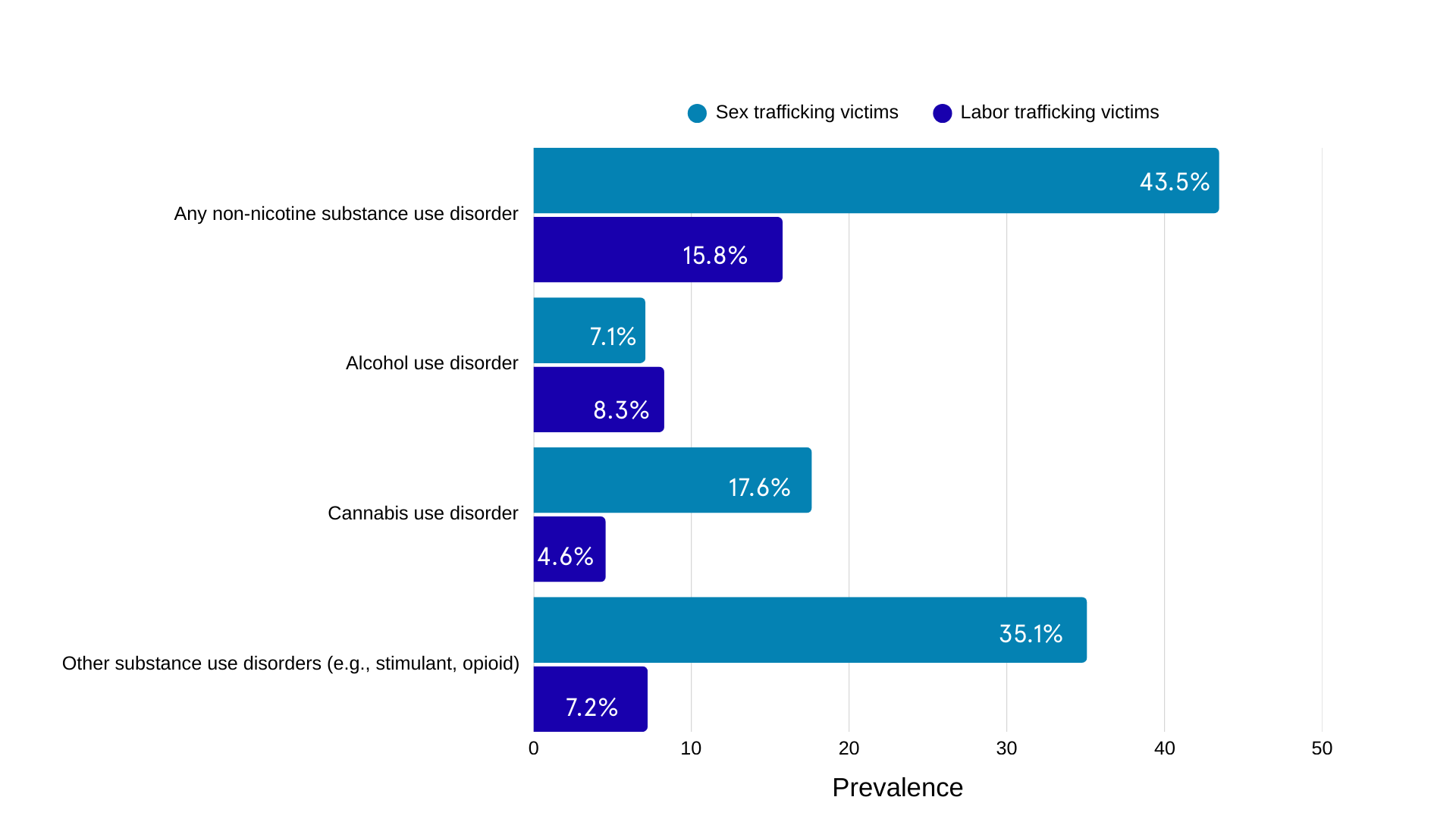
Figure. Prevalence of substance use disorders among sex trafficking victims and labor trafficking victims, as reported by Dell et al. (2025). Note: non-nicotine polysubstance use disorders are not included here because there were fewer than 10 cases among labor trafficking victims. Click image to enlarge.
Why do these findings matter?
There is a high need for SUD care among human trafficking victims presenting for care in ED. Healthcare providers can respond by routinely screening for SUDs among anyone suspected of being involved in human trafficking and facilitate linkages to trauma-informed SUD care, harm reduction services such as Narcan, and other needed mental or physical health services.
Every study has limitations. What are the limitations in this study?
The records used in this study offered only a snapshot in time and do not speak to how SUDs developed over the course of patients’ experience as victims of human trafficking. These findings should encourage more in-depth research into SUD development and recovery among these individuals.
For more information:
Help is available for people involved in human trafficking. For instance, in the US, the National Human Trafficking Hotline offers 24/7 confidential help. People who feel they need help for substance use problems can find information and help here or on our Addiction Resources page.
– Heather Gray, PhD
Want CE credit for reading BASIS articles? Click here to visit our Courses Website and access our free online courses.




