Editor’s Note: Today’s review is part of our month-long Special Series on Asian American/Pacific Islander (AAPI) Addiction Research. Throughout May, The BASIS is examining forms of addiction among AAPI communities.
Though the entire world felt the effects of the Covid-19 pandemic, some groups experienced significantly more adversity than others. For example, Asian American and Pacific Islanders experienced significantly higher rates of hospitalization due to Covid-19 compared to non-Hispanic whites. Environmental racism, lack of healthcare access, and rampant xenophobia towards Asian communities likely played a large part in driving these disparities. Discrimination can also lead to health problems such as substance misuse and other mental health issues. This week, as part of our Special Series on Asian American and Pacific Islanders, ASHES reviews a study by Andrew Subica and colleagues that examined the substance misuse patterns, mental health, and treatment needs of Native Hawaiian and Pacific Islanders (NH/PI) amidst the Covid-19 pandemic.
What was the research question?
What were the substance use patterns and mental health/treatment needs of NH/PIs amidst the Covid-19 pandemic, and were there any differences based on gender identity?
What did the researchers do?
This study involved 306 NH/PIs and purposefully oversampled non-binary NH/PIs, as this group is traditionally underserved. Participants completed a battery of assessments measuring alcohol use, tobacco use, illicit drug use, depression/anxiety, and behavioral health treatment needs. Participants who endorsed needing behavioral health treatment in the past 12 months were then asked whether they had ever avoided or delayed seeking such treatment. The researchers assessed prevalence rates and mean scores on these measures and used independent samples t-tests and chi-square analyses to compare differences between men and women NH/PIs.1
What did they find?
Though slightly less than half of participants (47%) reported current alcohol use, 17% reported past-month heavy episodic drinking and 27% screened positive for alcohol use disorder. While lifetime tobacco and cannabis use was fairly prevalent among the sample (~30%), other drug use was relatively rare (≤ 6%) and closer to estimates for the general population.2 Rates of major depressive disorder and generalized anxiety disorder were 27% and 19%, respectively, which are higher than the general population.3 Furthermore, 33% of participants reported needing behavioral health treatment in the past year; of these, 60% reported avoiding/delaying treatment. Finally, there were wide disparities based on gender identity, with non-binary NH/PIs reporting higher rates of nearly every outcome compared to women and men in the sample (see Figure). Notably, 44% of non-binary participants who needed behavioral health treatment avoided or delayed seeking it.
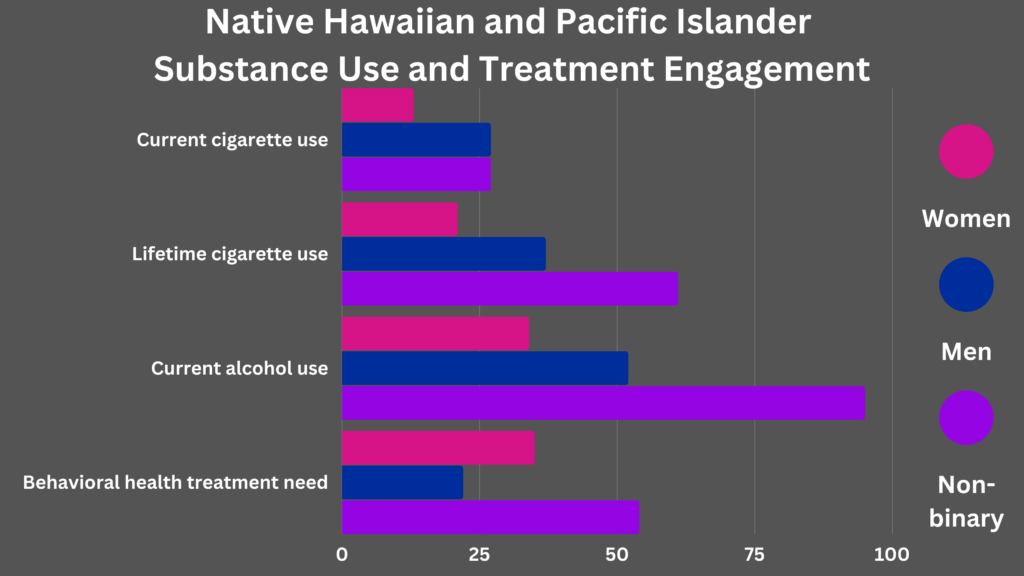
Figure. Displays the percentage of participants who endorsed each substance use category and behavioral health needs/delays, separated by gender identity. All differences between men and women were statistically significant though non-binary NH/PIs were excluded from these analyses. Click image to enlarge.
Why do these findings matter?
These findings provide insight into the health disparities experienced by NH/PI individuals. Through recognizing these disparities, we can begin to take action to reduce them. For example, now that we know a large proportion of NH/PIs who need behavioral health treatment have needed to delay such care, we can take action to improve the accessibility of such services. Additionally, this study shines a light on the importance of intersectionality. Though NH/PI individuals experience unique health disparities, many sub-groups, including NH/PIs who identify outside of the gender binary, experience compounding stigma due to their multiple marginalized identities. Improving the cultural competency of treatment services to better serve individuals with multiple stigmatized identities would undoubtedly improve treatment rates and success.
Every study has limitations. What are the limitations in this study?
This study lacked a comparison group so it is difficult to compare this population to other groups such as non-Hispanic whites or other minority groups. Comparisons to the general population relied on estimates from other studies that may have used different methods leading to imprecise comparisons. Additionally, this study collected data at only a single point in time so it is difficult to say how the pandemic affected NH/PI communities. Though it is likely that Covid-19 and the accompanying increase in racism worsened these outcomes, it is also possible that changes in social contact impacted substance use in ways that cross-sectional data cannot address.
For more information:
Asian Americans in search of mental health support may benefit from visiting Project Lotus. Others who are concerned about their substance use or mental health more generally may benefit from the Substance Abuse and Mental Health Services Administration’s resource finder. Additional resources can be found at the BASIS Addiction Resources page.
—John Slabczynski
What do you think? Please use the comment link below to provide feedback on this article.
________________
[1] The researchers also conducted several other analyses not covered in this review, including examining whether demographic and behavioral health variables were associated with alcohol use disorder and behavioral health treatment needs.
[2] For comparison, the general population prevalence in the United States during Covid-19 was 10.2% for alcohol use disorder, 13% for lifetime cigarette use, 3% for illicit opioid use, and 4% for methamphetamine use.
[3] For comparison, in the U.S. general population, 7.8% report major depressive episodes and 5% report generalized anxiety disorder.




