Methadone – a medication used to treat Opioid Use Disorder – is strictly regulated in the U.S. This medication can only be dispensed and administered by federally-certified opioid treatment programs (OTPs). Patients prescribed methadone are required to travel to an OTP, usually on a daily basis, to take their medication under the supervision of a physician. A shortage of OTPs nationwide, and in rural communities in particular, may create barriers to accessing this life-saving treatment. This week, STASH reviews a study by Paul J. Joudrey and colleagues that investigated the average drive time to the nearest OTP, in urban and rural counties in the 5 U.S. states with the highest county rates of opioid-related overdose mortality. For purposes of comparison, they also measured drive time to federally qualified health centers (FQHC) and dialysis centers. FQHCs are federally funded nonprofit health centers for medically underserved populations and provide primary care regardless of a patient’s ability to pay.
What were the research questions?
What is the average drive time to the nearest OTP, FQHC, and dialysis center in urban and rural counties in the 5 U.S. states with the highest county rates of opioid-related overdose mortality? What is the difference in average drive time to the nearest OTP vs. FQHC and OTP vs. dialysis center?
What did the researcher do?
The researchers used 2010 U.S. Census data to obtain the coordinates of the mean center of population for all counties in the 5 U.S. states with the highest county rates of opioid-related overdose mortality.1 Counties were classified into urban (large central metros, large fringe metros, medium metros, and small metros) and rural (micropolitan and noncore) categories based on the 2013 National Center for Health Statistics Urban-Rural Classification Scheme. The researchers calculated the minimum drive time (in minutes) from each county’s mean center of population to the nearest OTP, FQHC, and dialysis center. Drive times to the nearest OTP were compared with drive times to the nearest FQHC and dialysis center.
What did they find?
Two hundred seventy of the 487 counties were classified as rural. Included in this study were 109 OTPs, 952 FQHCs, and 837 dialysis centers. Across all counties, the average drive time to the nearest OTP was 37.3 minutes (see Figure). Drive times to OTPs were shortest in large central metro urban counties (7.8 minutes) and the longest in noncore rural counties (49.1 minutes). Across all counties, the average drive time to the nearest FQHC was 15.8 minutes and the average drive time to the nearest dialysis center was 15.1 minutes. On average, it took 21.5 more minutes to drive to an OTP compared to a FQHC and 22.1 minutes compared to a dialysis center. In all urban-rural county classifications, it took longer to drive to an OTP compared to a FQHCs or dialysis center.
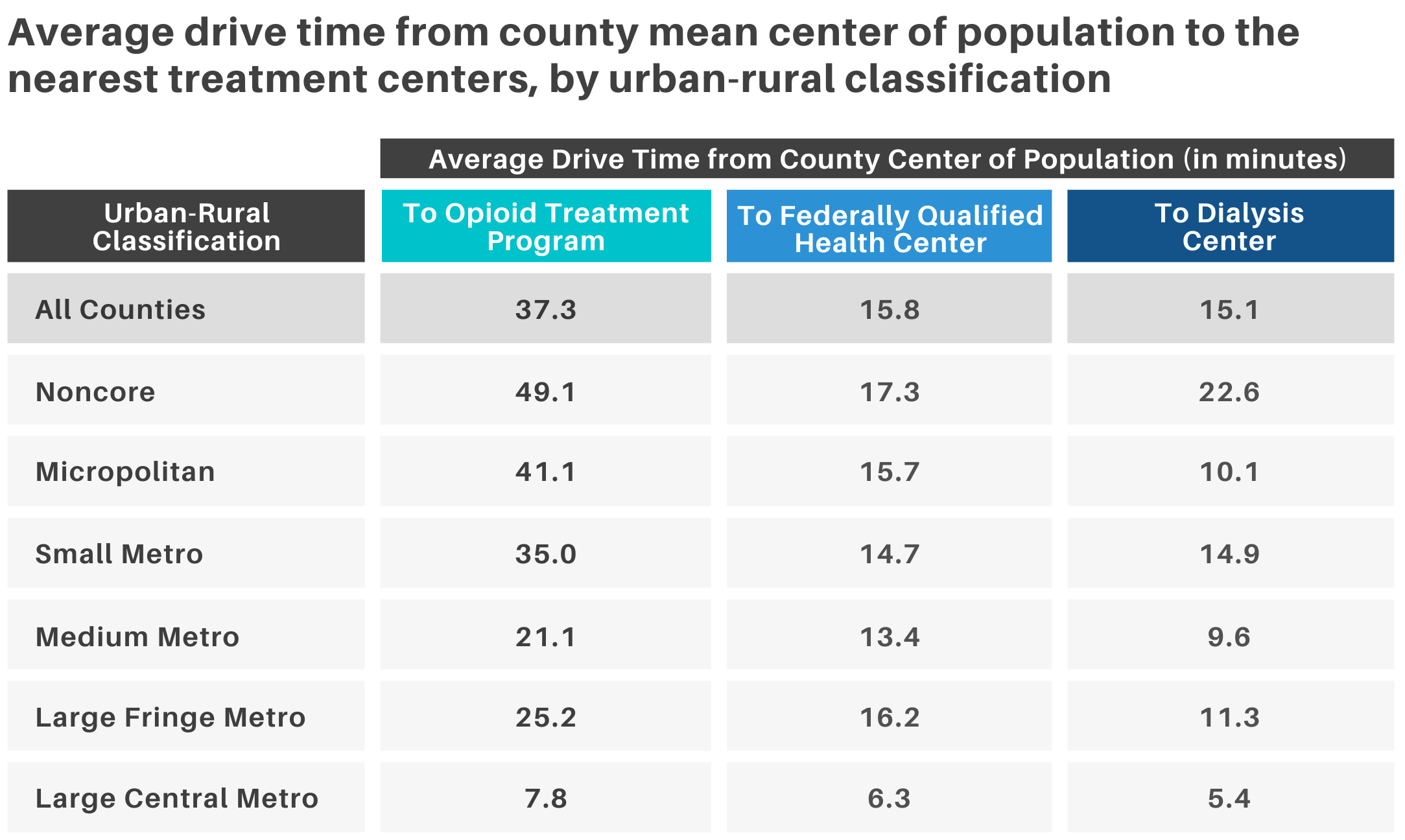 Figure. Average drive time (in minutes) from county mean center of population to the nearest treatment centers (opioid treatment program, federally qualified health center, and dialysis center), by urban-rural classification. Adapted from Joudrey et al. (2019). Click image to enlarge.
Figure. Average drive time (in minutes) from county mean center of population to the nearest treatment centers (opioid treatment program, federally qualified health center, and dialysis center), by urban-rural classification. Adapted from Joudrey et al. (2019). Click image to enlarge.
Why do these findings matter?
Rural communities face unique barriers to accessing treatment for Opioid Use Disorder. OTPs are less frequently found in rural areas compared to urban areas, and the facilities that do exist in these communities generally offer a limited array of services. As this study highlights, individuals in these communities often have to drive significant distances to the nearest OTP on a daily basis for their medication. This, along with a lack of reliable transportation, are common barriers to retention in methadone treatment among individuals in rural areas. Findings from this study demonstrate that drive times to FQHCs and dialysis centers are much shorter for rural communities compared to OTPs. Allowing FQHC providers to dispense and administer methadone might increase access to this treatment, especially for individuals in rural areas.
Every study has limitations. What are the limitations in this study?
Drive times calculated in this study were from the mean center of population; individual drive times within these counties vary. This study did not take into account public transportation and may overestimate travel time, especially in urban areas. This study was conducted before the COVID-19 pandemic, during which the U.S. Substance Abuse and Mental Health Services Administration is temporarily allowing OTPs to dispense up to a 28-day supply of take-home methadone.
For more information:
Are you worried that you or someone you know has an addiction? The SAMHSA National Helpline is a free treatment and information service available 24/7. For more details about addiction, visit our Addiction Resources page.
— Kira Landauer, MPH
What do you think? Please use the comment link below to provide feedback on this article.
________________
[1] The U.S. states with the highest county rates of opioid-related overdose mortality are Indiana, Kentucky, Ohio, Virginia, and West Virginia.