Supervised consumption sites (SCSs) are one of many harm reduction strategies intended to minimize the negative consequences associated with drug misuse. SCSs offer a controlled setting where people who use opioids can consume already-purchased drugs under supervision of trained staff who monitor for overdose, obtain sterile syringes and other materials, and receive referrals to health and social services. This week, STASH reviews a study by Jirka Taylor and colleagues that examined community attitudes about implementing SCSs for people who use opioids in four U.S. counties with high rates of opioid overdose deaths.
What were the research questions?
Do stakeholders believe that SCSs could help improve outcomes for people who use opioids? Do stakeholders believe SCSs would be acceptable to members of their community?
What did the researcher do?
The researchers conducted focus groups and key informant interviews with 159 stakeholders in four U.S. counties with high rates of opioid overdose deaths. Stakeholders included people who use opioids and those who interact with people who use opioids professionally (e.g., substance use treatment, medical, harm reduction, and social service providers, first responders, criminal justice and policy professionals). Interviewees and focus group participants were asked about their perspectives on current services and service gaps for people who use opioids, knowledge and opinions on the effectiveness of SCSs, opinions about the acceptability of SCSs to community members, and facilitators to increase SCS acceptability.
The researchers developed a list of themes that arose in the focus groups and during the key informant interviews. They examined the frequency of themes and how themes varied by stakeholder type (people who use opioids or those who professionally interact with people who use opioids). Theme frequency was reported as low (theme arose in 1-25% of transcripts), medium (26-50% of transcripts), high (51-75% of transcripts), or very high (76-100% of transcripts).
What did they find?
Stakeholders noted numerous benefits of SCSs for people who use opioids, including helping to prevent overdose deaths and providing linkages to treatment and other resources. People who use opioids, in particular, felt that SCSs could provide a safe and nonjudgmental space for them and could help prevent the spread of infections. At the same time, stakeholders expressed concerns. Many believed SCSs would be law enforcement traps and thought that stigma may deter people from using a SCS. Stakeholders, particularly people who use opioids, suggested that the desire to use drugs immediately after purchase might be a deterrent to traveling to a SCS. People who use opioids, particularly those currently in treatment, felt that SCSs would enable or perpetuate drug use.
Stakeholders felt that the implementation of SCSs would be impeded by the community values and local culture (see Figure), with conservative cultural beliefs, conservative politicians, fear and stigma, lack of awareness of the extent of the opioid epidemic, and overall resistance to harm reduction practices all contributing to potential resistance. Stakeholders, particularly those who do not use opioids, believed that SCSs were not seen as a priority in their community or might not be accepted in their community due to the belief that they may perpetuate or enable opioid use.
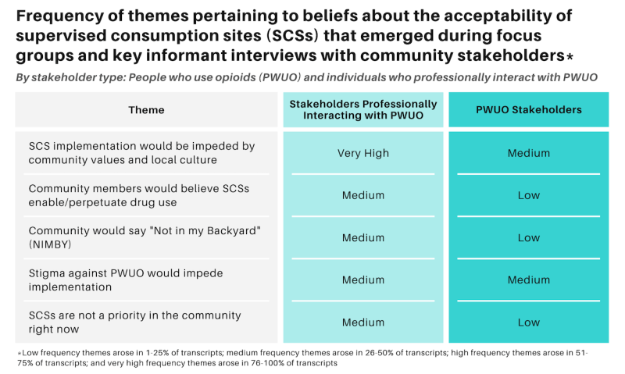
Figure. Frequency of themes pertaining to beliefs about the acceptability of SCSs that emerged during focus groups and key informant interviews with community stakeholders, by stakeholder type (people who use opioids stakeholders and stakeholders who professionally interact with people who use opioids). Click image to enlarge.
Why do these findings matter?
More than 120 SCSs are now operating globally and the first SCS in the U.S. opened in New York City in November 2021. As the U.S. looks to implement SCS in communities hit hardest by the opioid epidemic, it is important to understand community perspectives on acceptability of such programs. Findings from this study suggest that stakeholders in communities with high opioid overdose deaths generally recognize the benefits these facilities have for people who use opioids but that some degree of opposition to their implementation is expected. Educational campaigns might help correct some of the stigma and misinformation that feeds into lack of acceptability of SCSs, such as correcting the false belief that SCSs will increase drug use. To mitigate concerns about law enforcement traps, SCS should be run by existing, trusted entities in the community like syringe exchange programs.
Every study has limitations. What are the limitations of this study?
The study sample does not include the perspectives of all community stakeholders. In particular, it excluded politicians and business owners. Participants reflected on possible support or resistance from these other stakeholders but it is possible their views were not accurate. Findings from this study are not generalizable to other communities, such as counties with lower levels of opioid overdose deaths.
For more information:
Are you worried that you or someone you know has an addiction? The SAMHSA National Helpline is a free treatment and information service available 24/7. For more details about addiction, visit our Addiction Resources page.
— Kira Landauer, MPH
What do you think? Please use the comment link below to provide feedback on this article.