Editor’s Note: Today’s review is part of our month-long Special Series on Managing Addiction during COVID-19. Throughout September, The BASIS is highlighting how the COVID-19 pandemic has impacted people managing addiction. This Special Series is generously sponsored by the Greater Boston Council on Alcoholism.
The COVID-19 pandemic has disrupted people’s lifestyles and typical behaviors. In the United States, emergency department visits for mental health conditions, suicide attempts, all drug and opioid overdoses, intimate partner violence, and child abuse and neglect were higher in March-October 2020 compared with the same period in 2019. On the other hand, violent crimes and property crimes were lower for the first six months of 2020 than they were for the first six months of 2019. Driver behavior also changed with the implementation of stay-at-home guidelines and reductions in roadway travel. This week, STASH reviews a study by Jeremy Faust and colleagues that investigated whether the beginning of the COVID-19 pandemic affected the number of deaths due to drug overdose, homicide, unintentional injury, motor vehicle crash, and suicide in the United States.
What was the research question?
How did the first six months of the COVID-19 pandemic affect the number of deaths due to drug overdose, homicide, unintentional injury, motor vehicle crash, and suicide in the United States?
Author’s notes, Dr. Katherine Dickerson Mayes: “Throughout the pandemic, the media and general public have made predictions about the impact of COVID-19 on behavioral patterns. Our aim with this study was to quantify the expected vs. unexpected toll of various behavioral causes of death during the first six months of the pandemic.”
What did the researchers do?
Using monthly death counts published by the National Center for Health Statistics (NCHS), the researchers measured the number of observed deaths for March-August 2020. They used monthly death counts and US population data from January 2015-February 2020 to project the number of expected deaths for March-August 2020. Then, they calculated excess death by taking the difference between observed and expected deaths. They analyzed total excess death for all causes as well as excess death specifically due to the following external causes: drug overdose (intentional and unintentional), assault (homicide), unintentional injury, motor vehicle crash, and intentional self-harm (suicide). In addition, the researchers also estimated the percent of all non-COVID excess deaths that can be attributed to each of the five external causes.
What did they find?
From March-August 2020, there were over 250,000 total excess deaths, of which almost 175,000 had COVID-19 as the underlying cause. Compared to expected deaths, the number of observed deaths due to drug overdose, homicide, and unintentional injury were higher, motor vehicle crash deaths were about the same, and suicide deaths were lower (see Figure). Among non-COVID excess deaths, 12.7% were drug overdoses, 2.4% were homicide deaths, and 9.1% were deaths due to unintentional injuries.
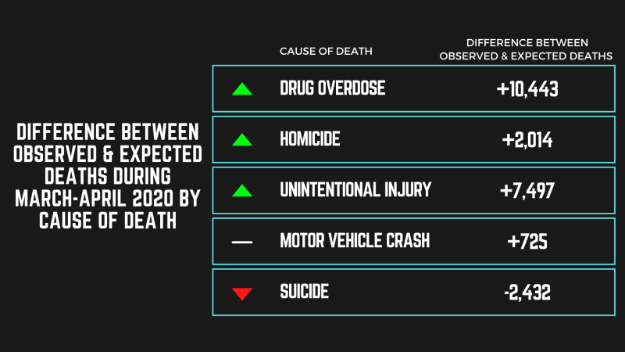
Figure. Difference between the number of observed and expected deaths during March-August 2020 for each of the five external causes: drug overdose, homicide, unintentional injury, motor vehicle crash, and suicide. Arrows indicate statistically significant results, with up arrows (green) indicating higher observed deaths than expected and down arrows (red) indicating lower observed deaths than expected. Click image to enlarge.
Why do these findings matter?
During the first six months of the COVID-19 pandemic, drug overdoses exceeded pre-pandemic trends, with over ten thousand more deaths than expected. Social isolation and unemployment stress may have led to increased drug use, and pandemic-related changes in treatment access possibly exacerbated mortality from overdoses. People with substance use disorder have been uniquely impacted by the pandemic, as they not only face threats from the COVID-19 virus itself but also from the effects of pandemic restrictions on their recovery. To meet the needs of this population, healthcare providers must adapt and develop new ways to deliver care, such as holding socially-distanced meetings under a tent or providing telehealth group-based opioid treatment.
Author’s notes, Dr. Katherine Dickerson Mayes: “Drug overdoses made up a sizable percentage of non-COVID excess deaths during this period (12.7%, 95% CI, 7.4% to 17.9%), though some of the increases were already apparent in the months directly before the pandemic. While the exact cause of this, whether it be diminished interpersonal support, limited access to social services, or increased mental health concerns, remains unclear, we feel this is an important area of future research and community action.”
Every study has limitations. What are the limitations in this study?
The 2020 data published by NCHS were considered preliminary at the time of analysis, though substantial changes in the data are unlikely. The monthly death counts were also based on death certificate data, which may have quality and accuracy issues, especially during emergencies.
For more information:
Substance use resources specific to COVID-19-related concerns can be found on the National Institute on Drug Abuse and Centers for Disease Control and Prevention websites. If you are worried that you or someone you know is experiencing addiction, the SAMHSA National Helpline is a free treatment and information service available 24/7. For more details about addiction, visit our Addiction Resources page.
— Caitlyn Fong, MPH
What do you think? Please use the comment link below to provide feedback on this article.