Primary care providers are uniquely positioned to address the opioid epidemic, from screening for opioid use disorder (OUD), to delivering harm-reduction interventions and providing evidence-based treatment. However, many providers harbor negative and stigmatizing attitudes and beliefs towards patients with OUD and other substance use disorders. This stigmatization deters individuals from seeking treatment and leads to substandard care. This week, STASH reviews a study by Jeffrey Schlaudecker and colleagues that examined if hearing personal narratives directly from individuals in active recovery positively impacts primary care provider attitudes and beliefs about persons with OUD.
What was the research question?
Does hearing personal narratives directly from individuals in active recovery positively impact primary care provider attitudes and beliefs about persons with OUD?
What did the researchers do?
The University of Cincinnati Department of Family and Community Medicine organized two professional development events for healthcare providers: (1) a half-day Community Opioid Summit with 154 attendees, and (2) a two-hour dinner discussion with 18 attendees. Attendees did not overlap. Both events consisted of educational sessions on topics related to the opioid epidemic, including personal narratives of patients in active recovery. In these sessions, individuals discussed their lived experience with OUD and their journey to recovery.
Summit presentations included: naloxone training/distribution, therapeutic communication to decrease stigma, inpatient management of acute opioid withdrawal, medication assisted treatment of OUD, a provider panel of addiction treatment facilities, and a semi-structured interview with a person in recovery detailing their lived experience with OUD. Dinner presentations included: opioid epidemic advocacy opportunities, a discussion of an article recounting a primary care doctor’s regret following a patient’s death from overdose, and discussions with persons in recovery about their experiences and the role primary care providers played in their personal journey from addiction to recovery.
After the event, attendees completed an anonymous survey evaluating self-reported attitudes and compassion using a four-point Likert scale. The researchers dichotomized responses into “strongly agree/agree” and “disagree/strongly disagree.” A follow-up survey was sent to Summit attendees two months after the event; open-ended responses were analyzed using thematic analysis.
What did they find?
Attendees identified the inclusion of patient voice as the most useful feature of the events (see Figure), and nearly all agreed that personal narratives told by individuals with lived experience were effective. Over 96% of Summit attendees and 100% of dinner attendees reported increased compassion for patients and families impacted by OUD, a deeper understanding of the challenges persons living with OUD face, and positive attitude change toward persons living with OUD. The value of patient voice and hearing real stories about addiction from real people emerged as an overarching theme from the open-ended survey questions. Attendees indicated that hearing from persons with lived experience challenged their assumptions and preconceptions about OUD and other substance use disorders.
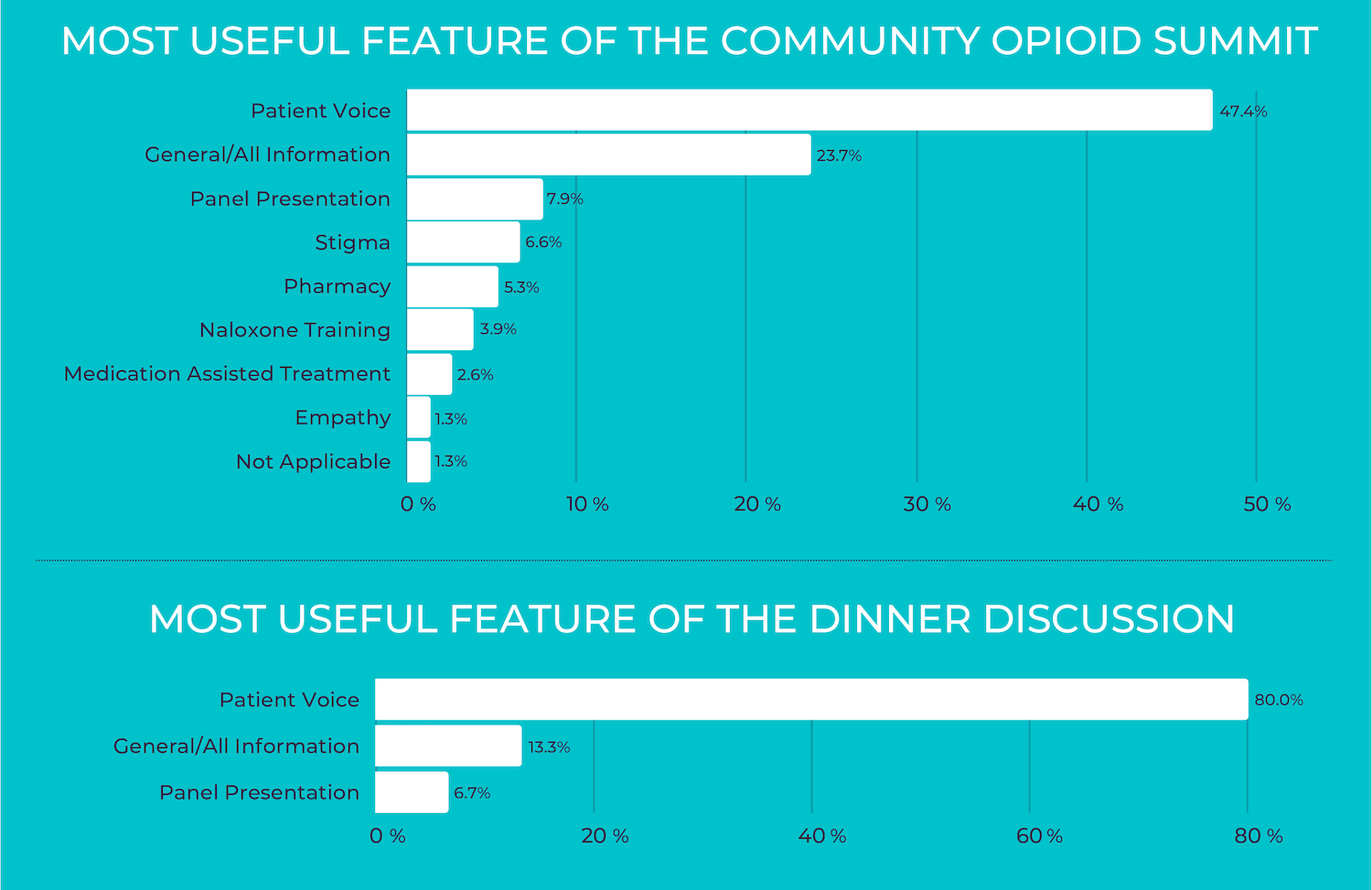
Figure. Most useful feature of educational sessions held during the professional development events. Percentages indicate the percent of attendees who identified the corresponding feature as most useful. Adapted from Schlaudecker et al. Click image to enlarge.
Why do these findings matter?
Interventions targeting healthcare professionals’ negative beliefs and attitudes towards substance use disorders are needed to reduce the stigmatization of persons living with these conditions. Contact-based interventions are one strategy for reducing stigma; they provide the opportunity for social contact between groups experiencing stigma and those who may be stigmatizing towards them. Findings from this study suggest incorporating contact-based interventions that amplify patient voice into provider education might be an effective strategy to improve negative and stigmatizing attitudes and beliefs. Medical school curricula, continuing medical education courses, and other professional development opportunities for healthcare providers should consider including patient voice when discussing addiction and other stigmatized conditions. Contact-based interventions might be utilized in conjunction with other evidence-based strategies to reduce stigma.
Every study has limitations. What are the limitations of this study?
This study relied on self-reported data; reported positive attitude change may be biased by social desirability. Attendance was voluntary meaning that the findings may be influenced by self-selection bias.
For more information:
Are you worried that you or someone you know has an addiction? The SAMHSA National Helpline is a free treatment and information service available 24/7. For more details about addiction, visit our Addiction Resources page.
— Kira Landauer, MPH
What do you think? Please use the comment link below to provide feedback on this article.