People who are in methadone maintenance treatment are at risk for problem gambling. Importantly, such patients are over 8 times more likely to dropout of methadone treatment and more likely to be using opioids during methadone maintenance treatment. Since these early studies, the gambling landscape has changed and new diagnostic tools have become available. This makes continued research important. Today on the WAGER, we review a study by Seth Himeloch and colleagues, which continues this line of research study.
What was the research question?
What is the nature of the gambling behavior and problems among those receiving methadone maintenance?
What did the researchers do?
Himelhoch and his colleagues recruited participants (n = 185) from an urban methadone maintenance program. They used the 9-item DSM-5 problem gambling criteria to assess prevalence of Gambling Disorder (GD). If participants endorsed 4 or more criteria, they qualified for a 12-month GD diagnosis. The researchers further classified participants as having mild (endorsed 4-5 criteria), moderate (6-7 criteria), or severe (8-9 criteria) Gambling Disorder. Himelhoch and his colleagues adapted questions from a previously used questionnaire to gather information about frequency of and money spent on various types of gaming and gambling behaviors.
What did they find?
Almost half (46.2%) of participants qualified for a GD diagnosis, and of these participants, 37% qualified for a severe GD diagnosis. The demographic characteristics (age, gender, race, income) of those with GD were not significantly different than participants without a GD diagnosis. Additionally, there was no difference in methadone dose. But, those that met criteria for GD had been in treatment for significantly less time. Participants with GD spent significantly more money each month on most types of gambling (see Figure).
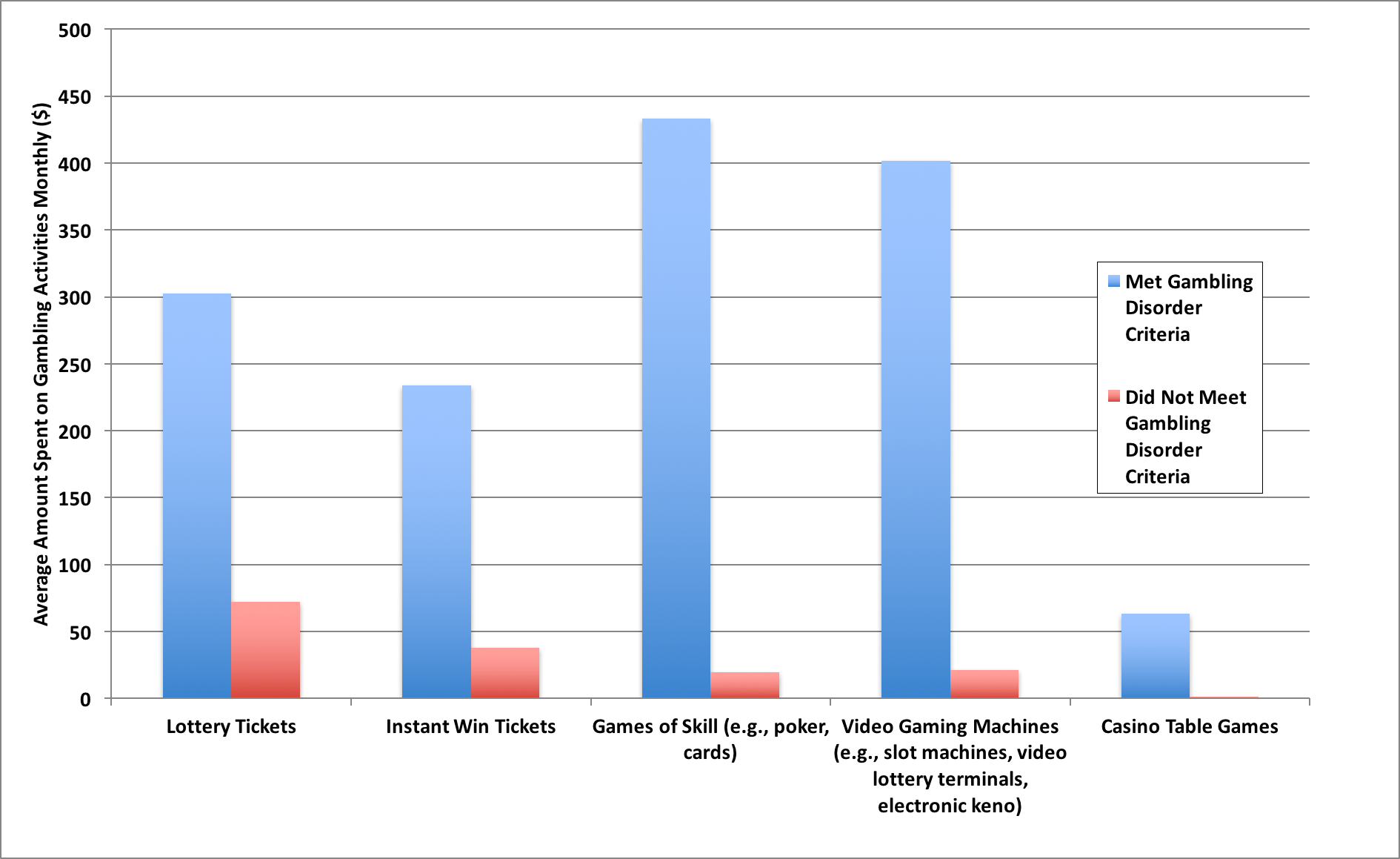 Figure. The average amount of money ($) methadone maintenance patients spend monthly on different types of gambling activities. Click image to enlarge.
Figure. The average amount of money ($) methadone maintenance patients spend monthly on different types of gambling activities. Click image to enlarge.
Why do these findings matter?
The prevalence of GD in this particular population, according to DSM-5 criteria, is substantially higher than that of a substance dependent population (10.3% met DSM-5 GD diagnosis) and that of the general population (0.6% met DSM-IV criteria for Pathological Gambling). Since previous research has found that people with GD have worse substance use treatment outcomes than those without GD, it may be important to screen for and treat GD symptoms in conjunction with opioid use disorder treatment. Previously, The BASIS has described a brief (3-question), validated screen for Gambling Disorder.
Every study has limitations. What were the limitations in this study?
This study population was predominantly African-American (71%) and recruited from an urban environment, and thus might not be generalizable to other populations receiving methadone maintenance treatment. This study was cross-sectional and therefore cannot comment on what caused what.
For more information:
Find the original publication abstract here. For more information regarding methadone maintenance, check out SAMHSA’s resources. Worried you or a loved one has a gambling problem? Check out the National Center for Responsible Gaming website for screening tools and resources.
— Layne Keating
What do you think? Please use the comment link below to provide feedback on this article.




Alan Feldman January 4, 2017
Is there any sense of whether the disordered gambling behavior was present before the start of methodone treatment or as a result of the treatment?
Ca January 4, 2017
In other words, when your character is weak, you are more likely to gamble your money away.
The BASIS January 5, 2017
Thanks for your question, Alan. Due to the cross-sectional nature of this study, it is difficult to comment on when the participants’ Gambling Disorder symptoms began. The questionnaire they used to determine GD prevalence specifically asks about symptoms within the previous 12 months. Since participants had been in treatment for an average of 3 years, it is plausible to assume participants had experienced GD symptoms concurrent with their treatment. The researchers, however, did not have any information on whether or not participants experienced symptoms of Gambling Disorder before their treatment began, and therefore cannot comment on any causal relationships. –Layne Keating
The BASIS January 5, 2017
Thanks for your comment, CA. Addiction is a complicated issue, and I believe those affected by it deserve our compassion. If you’re interested in understanding addiction, you might want to take a look at the Surgeon General’s recent report, available freely here: https://addiction.surgeongeneral.gov/surgeon-generals-report.pdf.
This statement, from pg. V of the report, sums up what science tells us about the nature of addiction:
“We also need a cultural shift in how we think about addiction. For far too long, too many in our country have viewed addiction as a moral failing. This unfortunate stigma has created an added burden of shame that has made people with substance use disorders less likely to come forward and seek help. It has also made it more challenging to marshal the necessary investments in prevention and treatment. We must help everyone see that addiction is not a character flaw – it is a chronic illness that we must approach with the same skill and compassion with which we approach heart disease, diabetes, and cancer.”
–Heather Gray
Celeste H January 7, 2017
This article is enlightening, and has provided valuable information. I currently treat individuals that receive medication assisted treatment (MAT), and several of my patients are struggling with GD. Some individuals seem to have replaced the fast lifestyle of opioid addiction with the “high” of purchasing scratch off tickets, or playing games of chance at the casino. They look forward to payday to engage in gaming, when before receiving MAT, they headed to the “spot” to use their drug of choice. Treating those with a propensity to engage in high risk behavior is challenging to say the least. Addiction, as you mentioned in the response to CA, is a chronic illness, a disease; no different than diabetes, or heart disease, and can be treated. However, as with any other disease, if the patient does not comply with the recommendations of their health professionals, change may not occur. I remain hopeful, as I’ve seen many individuals achieve goals, and live successful, productive lives while receiving MAT.
The BASIS January 9, 2017
Thank you for your comment, Celeste! We really appreciate you sharing your insight with us.
–Layne Keating