Evidence-based treatment should improve the quality of healthcare services by standardizing practices that have proof they are helpful. However, for many interventions, rigorous evaluation is not available for minority populations, such as Native Americans. The absence of multi-cultural evaluation of interventions risks the possibility that some approaches might not be a good fit for some populations. This week, as part of our special series on Addiction, Resilience, and Recovery within Tribal Communities, STASH explores this possibility by reviewing recent research on the use of evidence-based treatment in programs serving Native Americans.
What is the research question?
To what extent are substance use disorder treatment programs serving Native Americans using and approving of psychosocial evidence-based treatments?
What did the researchers do?
Douglas Novins and his colleagues completed a national survey of substance use disorder treatment programs servicing Native Americans. They used purposive stratified sampling to build their sample, recruiting 63% (N=192) of sites that they believed had the potential to provide substance use disorder treatment services to Native Americans. Treatment site representatives completed a survey that included questions related to their use of, and attitude toward, nine evidence-based psychosocial treatment practices for substance use disorder.
What did they find?
The five most commonly implemented psychosocial evidence-based practices were cognitive behavioral therapy, motivational therapy, relapse prevention therapy, twelve-step facilitation, and matrix model. Regression models suggested that providing evidence-based psychosocial treatment, more generally, was associated with receiving direct Indian Health Service funding, greater mean years of staff education, having certified addiction counselors on staff, requiring clinical use of evidence-based treatments, considering evidence-based treatments in strategic planning, and higher scores on a scale measuring openness to evidence-based treatments. A majority rated motivational interviewing and relapse prevention therapy as culturally appropriate; whereas, only a minority rated cognitive behavioral therapy, twelve-step facilitation, and matrix model as appropriate (see Figure 1).
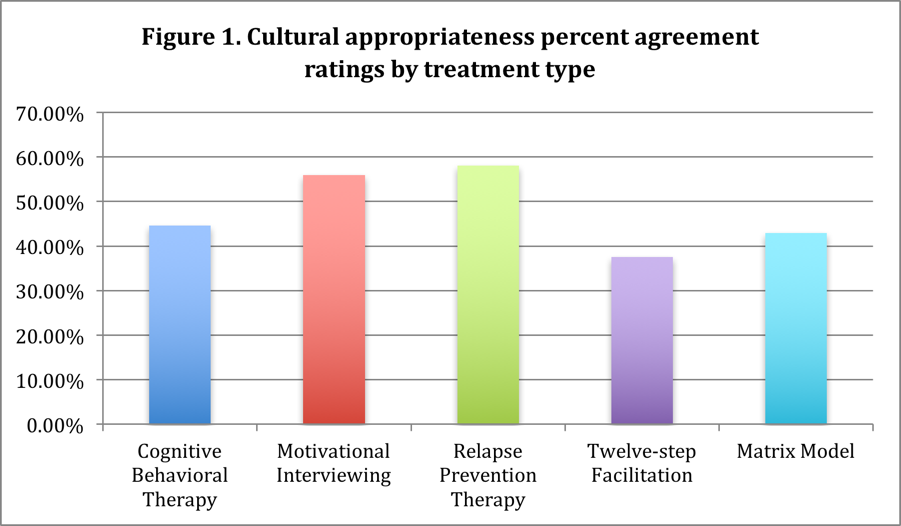
Figure. Click image to enlarge.
Why do these findings matter?
Although evidence-based treatments have the potential to provide substance use disorder intervention with high quality care options, neglecting to understand how such treatments might vary by population could limit their impact. Barriers to the use of evidence-based treatments and culturally inappropriate options could contribute to ongoing disparity problems for Native Americans. As treatments are developed, it is important to consider the diversity of individuals who might benefit from their use.
Every study has limitations. What about this one?
This study used a purposive sampling strategy that could overlook relevant programs, and limit its validity. Individuals represented organizations for this survey, and it is possible that respondent attitudes might be personal and not representative of organizational attitude, as a whole. As with many studies, self-report information is limited by response and memory biases.
For more information:
The Indian Health Service provides information for patients here.
–Debi LaPlante
What do you think? Please use the comment link below to provide feedback on this article.