For many, alcohol dependence (AD) is a multi-layered disorder. For these individuals, AD might co-occur with other mental health and/or substance use problems, such as opioid dependence. Research has shown that among people with AD, additional mental health and substance use problems likely contribute to risky behavior like driving under the influence. As part of our new Special Series on Opioid Dependence and Recovery, this week The DRAM reviews a study by Howard Moss and his colleagues that examines of the relationship between drug use, mental health disorders, and alcohol use patterns among those with AD.
What was the research question?
Is the severity and pattern of AD different for people with additional substance use and comorbid mental health problems?
What did the researchers do?
The researchers analyzed data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a survey of the general adult US population. Within that sample of approximately 40,000, 4% met past year DSM-IV criteria for alcohol dependence1. Moss and colleagues used latent class analysis to categorize these 1,172 into groups based on their self-reported past year substance use history.
What did they find?
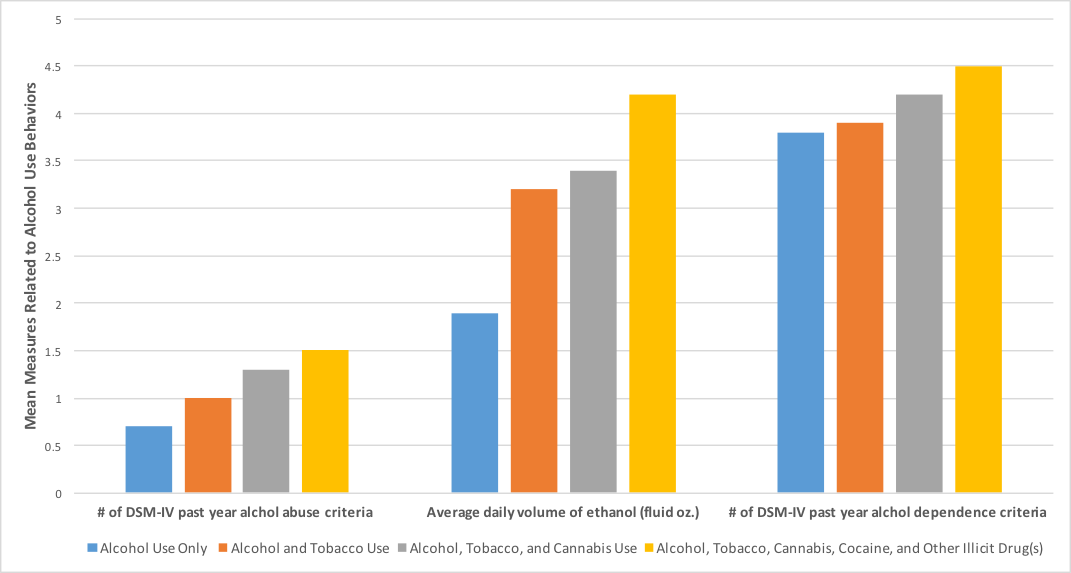
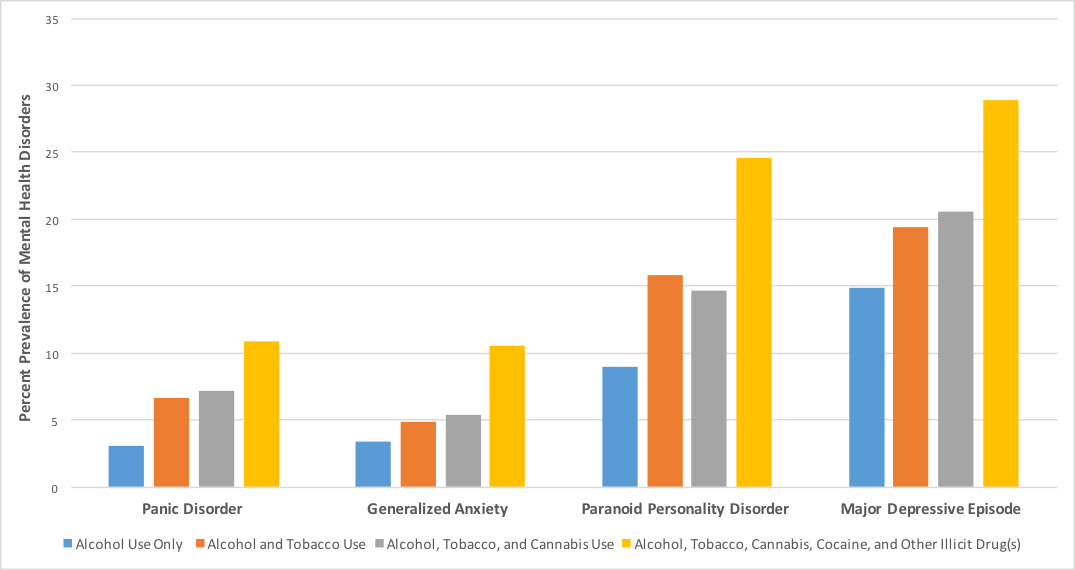
Latent class analyses identified four substance use groups among individuals with AD: (1) alcohol use only (30%), (2) alcohol and tobacco use (34%), (3) alcohol, tobacco and cannabis use (15%), and (4) alcohol, tobacco, cannabis, cocaine, other illicit drug(s) use (21%). Those in Group 4–the illicit polysubstance group– met more criteria for alcohol dependence and alcohol abuse and had more severe alcohol use behaviors than members of the other groups (Figure 1). The illicit polysubstance group also had the earliest age of onset for alcohol dependence and were the most likely to seek treatment. Finally, the illicit polysubstance group had a higher prevalence of some mood, anxiety and personality disorders than others (Figure 2).
Why do these findings matter?
Individuals with alcohol dependence without other substance use/mental health problems are only a small portion of the AD population, yet they are the most commonly represented in clinical trials and interventions. Treatment is then designed based on these trials, leaving those who struggle with AD in addition to other substance use/mental health problems with inadequate care. The current study suggests that treatment needs to evolve beyond the standard assessment and add layers of psychiatric and medical screening. As policy makers turn their attention to the epidemic of opioid dependence and overdose, they should keep in mind the complexity of challenges that may be prolonging and intensifying substance use disorders and associated consequences.
Every study has limitations. What about this one?
This study measured whether certain types of substance use and mental health issues co-occurred within the past year. However, the study cannot tell us whether participants used substances together or whether one kind of substance use or mental health problem was the particular cause of their alcohol dependence symptoms.
Figure 1. Alcohol use behavior among NESARC respondents with alcohol dependence
Figure 2. Prevalence of disorders among NESARC respondents with alcohol dependence
For more information:
If you or a loved one has a problem with alcohol or drugs please visit our first steps to change here.
— Alec Conte
What do you think? Please use the comment link below to provide feedback on this article.
Notes
1 The 4% prevalence rate for alcohol dependence relies on a complex weighting algorithm that accounts for the complex sampling design used in NESARC. Therefore, the 1,172 individuals analyzed in this paper are not exactly 4% of NESARC’s full sample.