Substance use and mental health disorders are serious concerns for veterans in the criminal justice system. Women in the criminal justice setting have a higher prevalence of drug use and mental health disorders than men. Unfortunately, due to a lack of research, it is unclear if this holds true for female veterans1. Recently, Andrea Finlay and her colleagues filled this knowledge gap by examining health records from the Veteran Health Association2.
What was the research question?
What is the prevalence of mental health and substance use disorders for female veterans in the criminal justice system?
What did the researchers do?
Finlay and her colleagues used records (2010-2012) from the Veterans Justice Outreach (VJO) program, associated with the Veterans Health Administration (VHA). They examined the demographics, mental health and substance use disorder diagnoses, and related treatment entry of 30,478 male and 1535 female veterans. The VJO program meets with veterans entering the criminal justice system in settings like courts or jail, focusing on addressing any health care or mental health needs they may have. The researchers analyzed data from veterans who visited a VHA facility within a year of their VJO visit, where they received a mental health or substance use disorder diagnosis if applicable.
What did they find?
Female veterans were more likely to be diagnosed with a mental health disorder (88%), specifically PTSD and depressive, bipolar, anxiety, and personality disorders, than male veterans (76%). Female veterans, however, were less likely to be diagnosed with a substance use disorder (58%) compared to male veterans (72%). The authors report that these rates are higher than that of either the criminal justice or veteran population alone, but may not be comparable due to different data collection methods. Among all veterans diagnosed with a mental health disorder, women were less likely to access residential mental health treatment than men.
Why do these findings matter?
Female veterans in the criminal justice system are less likely to utilize residential treatment despite having a greater likelihood of a mental health problem than male veterans. Because female veterans made up only 4% of the studied sample, it is possible that a lack of specialized VHA resources is both a contributing factor and a potential roadblock to addressing this discrepancy. And, specialized resources are necessary. Female veterans were more likely to have a service-connected disability and were more likely to experience military sexual trauma3. These findings suggest that the VHA needs to improve and expand their resources for female veterans, particularly those in the criminal justice system.
Every study has limitations. What were the limitations in this study?
The sample included veterans involved in the VJO program and therefore excluded veterans that already were incarcerated or not involved with the program. Future research is necessary to understand the relationships of mental health and substance use for all male and female veterans in the criminal justice system.
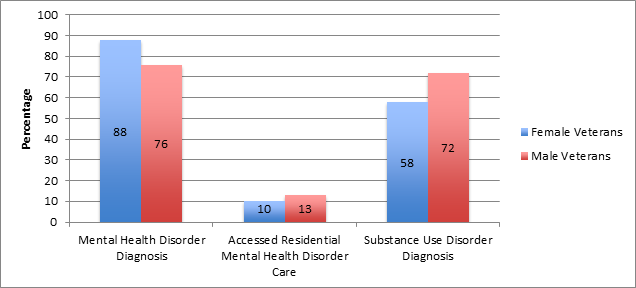
Figure. The percentage of female and male veterans who (1) were diagnosed with a mental health disorder, (2) accessed residential mental health treatment, and (3) were diagnosed with a substance use disorder. Click image to enlarge.
For more information:
Find the original publication abstract here.
For more information on the Veterans Justice Outreach Program or contact information for services in your area, click here.
Here are some resources specific for female veterans.
— Layne Keating
What do you think? Please use the comment link below to provide feedback on this article.
________________
[1] Binswanger, I. A., Merrill, J. O., Krueger, P. M., White, M. C., Booth, R. E., & Elmore, J. G. (2010). Gender differences in chronic medical, psychiatric, and substance-dependence disorders among jail inmates. American Journal of Public Health, 100(3), 476–482.
[2] Finlay, A. K., Binswanger, I. A., Smelson, D., Sawh, L., McGuire, J., Rosenthal, J., … Frayne, S. (2015). Sex differences in mental health and substance use disorders and treatment entry among justice-involved Veterans in the Veterans Health Administration. Medical Care, 53(4 Suppl 1), S105–111.
[3] Kimerling, R., Street, A. E., Pavao, J., Smith, M. W., Cronkite, R. C., Holmes, T. H., & Frayne, S. M. (2010). Military-related sexual trauma among Veterans Health Administration patients returning from Afghanistan and Iraq. American Journal of Public Health,100(8), 1409–1412.




