Bariatric surgery is often proposed as a treatment for severe obesity. More than 200,000 such procedures are performed in the United States each year (Elliott, 2012). Some bariatric procedure patients notice an increased sensitivity to alcohol after surgery, potentially because the procedure causes alcohol to be absorbed faster (Klockhoff, Naslund and Jones, 2002). In this issue of the DRAM, we review a study that investigates a possible link between bariatric surgery and alcohol use disorder (King et al., 2012).
Methods
- King et al. (2012) recruited 4,476 patients, age 18 or older, between February 2006 and February 2009 who were seeking a first bariatric procedure at one of 10 centers in the United States.
- The participants were asked to complete the Alcohol Use Disorder Identification Test (AUDIT) before the procedure, one year after the procedure, and two years after the procedure.
- Patients (n = 1,945) who were included in the dataset (1) completed the AUDIT before the procedure, (2) underwent the procedure, and then (3) completed the AUDIT again at least once after the procedure.
- Researchers tested models predicting post-procedure alcohol use disorder (AUD) from pre-procedure substance use behaviors and other psychosocial variables.
Results
- The proportion of participants qualifying for AUD was significantly higher in the 2nd year post-procedure than either pre-procedure or in the 1st year post-procedure (see Figure).
- Almost two-thirds (62.3%) of those who qualified as having an AUD before their procedure also qualified for an AUD sometime in the two years after the procedure. Eight percent (7.9%) of those who did not qualify for an AUD pre-procedure qualified for an AUD in the two years after the procedure.
- Statistically significant predictors for having an AUD post-procedure included:
- Pre-procedure AUD (odds ratio [OR] = 4.5 at age 20; OR = 11.14 at age 45);
- Male gender (OR =2.14);
- Pre-procedure Smoking (OR = 2.58);
- Pre-procedure regular alcohol consumption (at least 2 drinks per week) (OR = 6.37);
- Pre-procedure recreational drug use (OR = 2.38);
- Outcome two years after procedure, rather than one year (OR = 1.57).
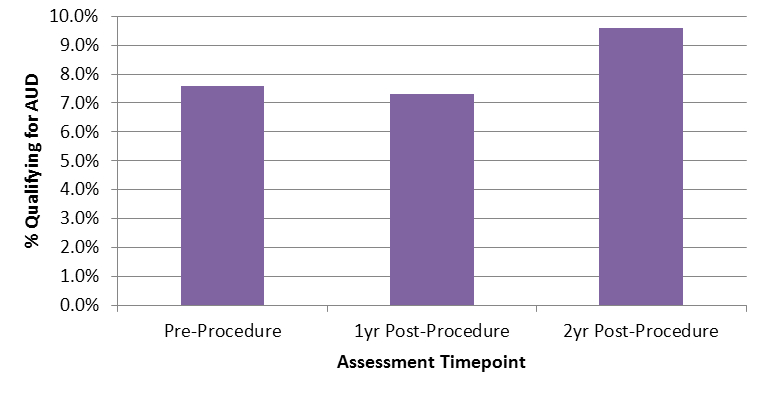
Figure. AUD Prevalence before, 1 year after, and 2 years after bariatric procedure. Note: Percents are based on the 1,389 participants who responded to the relevant questions on the AUDIT at all three time periods (before procedure, one year after procedure, and two years after procedure). 2yr Post-procedure prevalence significantly different than other two time points, p < .01. Click image to enlarge.
Conclusion
This study investigated alcohol use disorder rates in bariatric surgery patients both before and after surgery. One important finding was that the prevalence of AUD two years after surgery was greater than the prevalence rate one year after surgery. Future studies should continue to investigate the longer-term effects of bariatric surgery. Clearly, not all patients who undergo bariatric procedures go on to develop AUD; future research should also examine factors that increase or decrease risk among this population.
-Matthew Tom
What do you think? Please use the comment link below to provide feedback on this article.
References
Barbor, T.F., Higgins-Biddle, J.C., Saunders, J.B., and Monteiro, M.G. (2001). AUDIT The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. 2nd ed. Geneva, Switzerland: World Health Organization.
Elliott, V.S. (2012, April). Bariatric surgery maintains, doesn’t gain. American Medical News, http://www.ama-assn.org/amednews/2012/04/23/bisa0423.htm.
King, W.C., Chen, J.Y., Mitchell, J.E., Kalarchian, M.A., Steffen, K.J., Engel, S.G., Courcoulas, A.P., Pories, W.J., and Yanovski, S.Z (2012). Prevalence of alcohol use disorders before and after bariatric surgery. Journal of the American Medical Association, 307 (23), 2516-2525.
Klockhoff, H., Naslund, I. and Jones, A.W. (2002). Faster absorption of ethanol and higher peak concentration of women after gastric bypass surgery. British Journal of Clinical Pharmacology, 54 (6), 587-591.