Many of the veterans returning from Afghanistan and Iraq have survived injuries typically fatal during past wars. As such, larger portions of the veteran population are experiencing high levels of physical and psychological pain. Opioid medication is very effective at alleviating pain symptoms, but it carries risks of dependence, injury, overdose, and death. Thus, it is crucial to understand how veterans experience their pain relief treatment. This week’s STASH reviews a study that examines opioid prescription practices for veterans, with a focus on how co-morbid mental health conditions impact opioid treatment experience (Seal, Shi, Cohen, Cohen, Maguen, Krebs et al., 2012).
Methods
The study cohort originated from the Veterans Affairs (VA) roster of Operation Enduring Freedom and Operation Iraqi Freedom veterans.
- The study retrospectively examined veterans who entered the VA healthcare system between Oct 1, 2005 and Dec 31, 2008 (N=291,205)
- For the results reported here, the authors focused on veterans who received a new non-cancer diagnosis that could result in pain within 1 year of VA entry (N=141,029)
- Using data obtained from VA databases, the authors examined medical care and outcomes for 1 year following non-cancer diagnosis.
- The researchers divided the cohort into three groups:
- Veterans with no mental health diagnosis (49 % of the sample)
- Veterans with mental health diagnoses not including PTSD (19% of the sample)
- Veterans with a PTSD diagnosis with or without another mental health diagnosis (32% of the sample).
- The authors measured opioid prescriptions, including duration and dosage, as well as adverse clinical outcomes (e.g., accidents resulting in wounds or injuries, opioid-related accidents and overdoses, and self-inflicted injuries).
Results
- Although 6.5% of veterans without a mental health diagnosis were prescribed opioids, 11.7% of those with a mental health diagnosis other than PTSD and 17.8% of those with a PTSD diagnosis were prescribed opioids. Of the sub-group of patients with a PTSD diagnosis, those with co-morbid substance use disorders were especially likely to be prescribed opioids. (See Figure.)
- Among those who were prescribed opioids, veterans with PTSD experienced higher-risk treatment compared to veterans without mental health diagnoses. Compared to those without a mental health diagnosis, those with PTSD were
- More likely to be part of the group prescribed the highest quintile dose of opioids (22.7% vs. 15.9%; adjusted relative risk = 1.42)
- More likely to be prescribed opioids for longer than 2 months (63.2% vs. 42.7%; adjusted relative risk, 1.47)
- More likely to receive multiple opioids (19.8% vs. 10.7%; adjusted relative risk, 1.87).
- Veterans who were prescribed opioids had a higher rate of experiencing any adverse clinical outcome than those who were not prescribed opioids (9.5% vs. 4.1%; adjusted relative risk: 2.33).
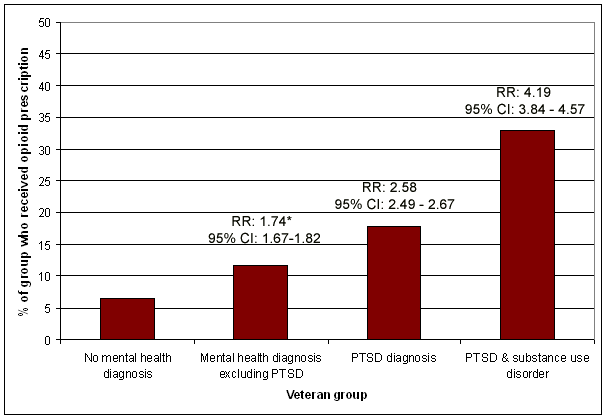
Figure. Rates of receiving an opioid prescription among the veteran groups. * adjusted relative risk compared with the group with no mental health diagnosis. The group of veterans with PTSD and substance use disorder is a sub-group of the group of veterans with PTSD. Click image to enlarge.
Limitations
- The VA administrative databases lacked variables such as education and level of combat exposure. As a result, potential confounding variables could be missing.
- The study did not have information concerning non-prescription opioid use or prescriptions outside of the VA system.
- Some of the adverse clinical outcomes might have occurred after veterans discontinued their prescription opioid use.
- The specific inclusion criterion of VA veterans with a non-cancer pain diagnosis means that the sample might not be representative of all veterans.
Conclusions
Veterans with a mental health diagnosis experienced higher-risk opioid treatment compared to those without such a diagnosis; this was especially true for veterans with PTSD. This treatment experience was associated with adverse clinical outcomes. The authors speculate that veterans with a mental health condition, especially PTSD, present to their primary care providers with greater pain levels, potentially because they experience psychological pain as physical pain, or because their endogenous pain control systems are not functioning well. These results suggest that it might be useful to provide more training to VA primary care providers and revisit opioid treatment practices for veterans who present with mental health issues.
-Jed Jeng
What do you think? Please use the comment link below to provide feedback on this article.
References
Seal, K. H., Shi, Y., Cohen, G., Cohen, B. E., Maguen, S., Krebs, E. E., et al. (2012). Association of mental health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and Afghanistan. Journal of the American Medical Association, 307(9), 940-947.