Past research shows that problem gambling shares many neuropsychological similarities with substance use disorders: people with problem gambling show evidence of withdrawal and tolerance, and their brains demonstrate activity similar to that of people addicted to illicit substances (Breiter & Gasic, 2003; Shaffer et al., 2004; Wray & Dickerson, 1981). This week the WAGER reviews a study that examined similarities in decision-making deficits between people with problem gambling and people with alcohol dependence (Lawrence, Luty, Bogdan, Sahakian, & Clark, 2009).
Methods
- The investigators recruited:
- Problem Gamblers (PGs): a community sample (n=21) of male problem gamblers (>=3 on the South Oaks Gambling Screen [SOGS]);
- Alcohol Dependent Individuals (ADs): male outpatients with alcohol dependence (n = 21);
- Healthy Controls (HCs): a community sample (n=21) of healthy male controls (<=2 on the SOGS).
- Participants completed a battery of neuropsychological tests that assessed:
- Decision-making and wagering in risky situations (the Cambridge Gamble Task);
- Tendency to act impulsively vs. gather extra information (the Information Sampling Test); and
- Working memory (the CANTAB Spatial Working Memory Test and the Digit
Span Test).
Results
- Table 1 displays the results for PGs, ADs, and HCs.
- PGs wagered more and were more likely to experience bankruptcies than controls on the CGT; they also made more errors than controls on the IST. PGs did not differ significantly from ADs on these assessment outcomes.
- PGs and ADs opened fewer boxes than controls in the IST, indicating greater impulsivity.
- ADs demonstrated working memory deficits compared to controls and PGs on both the SWM test and the DS test, and took longer than controls and PGs to make decisions in the CGT.
Table 1 – Neurocognitive Assessment Scores (adapted from Lawrence et al., 2009)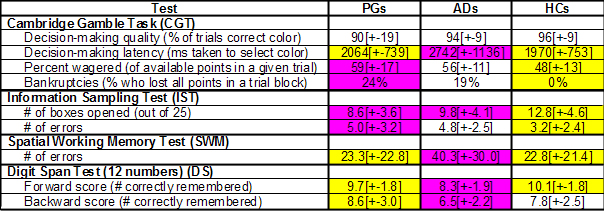
Note. PGs = Problem gamblers; ADs = Alcohol dependent individuals; HCs = Healthy controls. Cells highlighted in pink are statistically different from those highlighted in yellow (p < .05). Pink indicates a decision-making deficit.
Limitations
- The study examined only male participants.
- The study recruited ADs from a treatment program, but recruited PGs from the community, somewhat limiting comparability.
- The study cannot establish whether decision-making deficits preceded or resulted from addictive behavior.
Conclusion
PGs and ADs appear to share deficits in impulsive decision-making (i.e., deficits on the IST), and to some extent, risky decision-making (i.e., wagering behavior on the IGT). Only ADs experienced working memory deficits. Prior research suggests that the working memory deficits experienced only by the ADs in this study might be a neurological consequence of heavy alcohol use (e.g., Sullivan, Rosenbloom, & Pfefferbaum, 2000). The other deficits likely represent shared neurological vulnerabilities for both gambling and alcohol use problem. Future research will need to test this causal interpretation.
-Sarah Nelson
What do you think? Please use the comment link below to provide feedback on this article.
References
Breiter, H. C., & Gasic, G. P. (2003). A general circuitry processing reward / aversion information and its implications for neuropsychiatric illness. In M. Gazzaniga (Ed.), The cognitive neurosciences (3rd ed.). Boston: MIT Press.
Lawrence, A. J., Luty, J., Bogdan, N. A., Sahakian, B. J., & Clark, L. (2009). Problem gamblers share deficits in impulsive decision-making with alcohol-dependent individuals. Addiction, 104(6), 1006-1015.
Shaffer, H. J., LaPlante, D. A., LaBrie, R. A., Kidman, R. C., Donato, A. N., & Stanton, M. V. (2004). Toward a syndrome model of addiction: Multiple expressions, common etiology. Harvard Review of Psychiatry, 12, 367-374.
Sullivan, E. V., Rosenbloom, M. J., & Pfefferbaum, A. (2000). Pattern of motor and cognitive deficits in detoxified alcoholic men. Alcoholism: Clinical and Experimental Research, 24, 611-621.
Wray, I., & Dickerson, M. G. (1981). Cessation of high frequency gambling and "withdrawal' symptoms. British Journal of Addiction, 76(4), 401-405.




Charles Vorkoer September 29, 2010
There was a question that seemed pressing in this report: what is meant by “impulsive?” Is this a character issue? an aspect of being dissociated or in a state resembling hypnosis? Is this a drug brought into the body? Is this a fixed state? It seems to me that these variables would be very clinically important over a definition of “impulsive” as defined as some non-consideration of consequences or not thinking about choices.