The sharing of syringes for injection drug use (IDU) can lead to a variety of diseases: hepatitis B (HBV); hepatitis C (HCV); and Human Immunodeficiency Virus (HIV). One successful public health intervention to combat the repeated use of potentially contaminated syringes is a syringe exchange program (SEP) (e.g., Des Jarlais & Friedman, 1998). In countries such as Australia and the United Kingdom, the federal government provides funding to help support SEPs (Des Jarlais et al., 2006). In the United States, because some politicians believe funding SEPs supports drug use (Christoffersen, 2007), the federal government currently prohibits federal funding for SEPs. However, 36 states (“Syringe exchange programs–United States, 2005”, 2007) and a variety of private entities fund SEPs across the U.S. This week’s STASH reviews a recent study by Neaigus et al. (2008), which investigated injection drug users’ source of syringes, risky IDU behaviors, and rates of blood born diseases within two communities: New York, NY (NYC) where SEPs are allowed, and Newark, NJ where SEPs are prohibited under state law.
Utilizing a cross-sectional study design, researchers interviewed 526 injection drug users (IDUs) not currently in treatment that had used drugs during the past 30 days. Researchers recruited participants using targeted street outreach programs and by asking participants to nominate injection drug using friends. Interviewers inquired about socio-demographic information, injection drug use, drug treatment history, risky IDU behaviors, and syringe source. After the interview, phlebotomists conducted blood tests to determine HIV, HBV, and HCV status. Researchers conducted multivariate logistic regression controlling for potential confounders (e.g. race/ethnicity and years since initiated injecting) to determine adjusted odds ratios of blood infections, syringe sources, and injecting risk behaviors for each city.
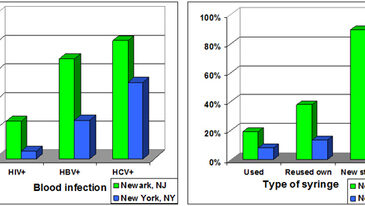
Figure. Percent of participants with blood infections & percent of participants who utilized risky injecting behaviors in the past 30 days (adapted from Neaigus et al., 2008). Click image to enlarge.
The left side of Figure 1 shows that 26.1% of injection drugs users in Newark, NJ tested positive for HIV compared to 5.2% in NYC. In addition, 69.6% of IDUs from Newark tested positive for HBV and 82.4% tested positive for HCV compared to 27.1% of IDUs in NYC who tested positive for HBV and 53.4% for HCV. The right side of Figure 1 shows that 19.2% of IDUs in Newark, NJ used another person’s previously used syringe to inject compared to 8% in NYC. In Newark, NY 37.9% of IDUs reused their own syringes when injecting compared with 13.5% in NYC. Finally, 89.7% of IDUs in Newark reported not always injecting only once with a new, sterile syringe that had been sealed in a wrapper compared with 59.9% in NYC.
This study might suffer from the ecological fallacy; associations observed at the population level do not mean an association exists at the individual level. In other words, the differences observed between IDUs in Newark, NJ and New York, NY might not be related to the legality of SEPs in the two cities. For example, rates of HIV between the two cities might be unrelated to the legality of SEPs, but due to a variety of factors at the individual level (e.g. sexual practices) that researchers did not measure. Besides the blood tests for infection, all other responses are self-report, which might lead to over-reporting of positive behavior. In addition, the cross-sectional design does not allow researchers to determine causality, that is, they cannot identify the temporal relationship between behaviors related to syringe use and infection.
Despite these limitations, this study suggests that both the federal and state governments should legalize and support SEPs. SEPs eliminate the need for IDUs to purchase syringes from unsafe sources and reusing and/or sharing syringes, reducing rates of HIV, HBV, and HCV infection. SEPs also provide an opportunity for public health advocates to provide IDUs with other forms of prevention (i.e. pamphlets, safe sex materials, and brief counseling). Both the federal and state governments should reexamine laws restricting SEPs because both are responsible for treating IDUs suffering from infection and because the cost of treating HIV, HBV, and HCV is much more than the cost of preventing infection.
What do you think? Please use the comment link below to provide feedback on this article.
References
Christoffersen, J. (2007). Needle exchange programs struggle with funding despite positive studies [Electronic Version]. USA Today. Retrieved May 12, 2008 from http://www.usatoday.com/news/health/2007-03-11-needleexchange_N.htm.
Des Jarlais, D. C., & Friedman, S. R. (1998). Fifteen years of research on preventing HIV infection among injecting drug users: what we have learned, what we have not learned, what we have done, what we have not done. Public Health Rep, 113 Suppl 1, 182-188.
Des Jarlais, D. C., Sloboda, Z., Friedman, S. R., Tempalski, B., McKnight, C., & Braine, N. (2006). Diffusion of the D.A.R.E and syringe exchange programs. Am J Public Health, 96(8), 1354-1358.
Neaigus, A., Zhao, M., Gyarmathy, V. A., Cisek, L., Friedman, S. R., & Baxter, R. C. (2008). Greater Drug Injecting Risk for HIV, HBV, and HCV Infection in a City Where Syringe Exchange and Pharmacy Syringe Distribution are Illegal. Journal of Urban Health: Bulletin of the New York Academy of Medicine.
Syringe exchange programs–United States, 2005. (2007). MMWR Morb Mortal Wkly Rep, 56(44), 1164-1167.