Psychiatric comorbidity is elevated among people guilty of driving under the influence of alcohol (DUI; Lapham et al., 2001). Consequently, understanding the psychiatric profiles of repeat DUI offenders is important for developing and delivering effective treatment (Nelson et al., 2007). This week’s DRAM presents epidemiological information about the frequency of psychiatric disorders among repeat DUI offenders attending a treatment program compared to the general US adult population (Shaffer, Nelson, LaPlante, LaBrie, & Albanese, 2007).
Massachusetts’ judges can offer adults who have received two or more DUI convictions participation in a two-week inpatient treatment program as an alternative to incarceration. As part of the program’s intake procedure, trained counselors administer a truncated version** of the Composite International Diagnostic Interview (CIDI) to all eligible admissions (i.e., those who spoke English and had no cognitive difficulties). The CIDI is a comprehensive, standardized, and computer guided instrument to assess interviewees for the presence of substance use and other mental disorders according to ICD-10 and DSM-IV criteria. The investigators compared the psychiatric profiles of 729 eligible and consenting consecutive admissions during a period of 15 consecutive months (79% of eligible admissions) to data from the National Comorbidity Survey Replication (NCS-R; Kessler, Berglund, Demler, Jin, & Walters, 2005). The NCS-R used the same version of CIDI to survey a nationally representative household sample of adults (N = 9,282).
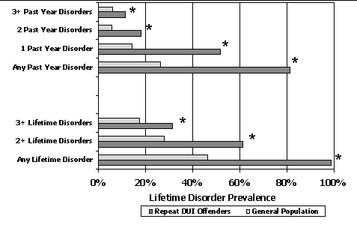
The sample was 81% male, 88% Caucasian, and the average age was 39.7 (SD = 11.6). Thirty-two percent had an income lower than $20,000, 72% had a high school education or less, 63% were employed, and 97.6% qualified for a substance use disorder during their lifetime. The Figure shows the prevalence of 1, 2, and 3 or more different disorders occurring during participants’ lifetime and within the past year. The DUI treatment population consistently had a significantly greater likelihood of disorder than the general population.
Figure. Comparing the prevalence of psychiatric comorbidity between repeat DUI offenders and a general population community sample (adapted from Shaffer, Nelson, LaPlante, LaBrie, & Albanese, 2007). Click image to enlarge
Note: Includes only disorders measured by both this study and the NCS-R.
*p<.001
One limitation of the Shaffer et al. study is that the study sample might not generalize to all repeat DUI offenders in Massachusetts or elsewhere. The treatment program only served 53% of those repeat offenders who were sentenced to treatment and agreed to that option instead of prison time. Therefore, those who did not attend this program might have a different diagnostic profile of addictive and psychiatric disorders. Furthermore both the DUI treatment group and the NCS-R group self-reported psychiatric symptoms, which might reflect a reporting bias.
Despite these limitations, these results demonstrate that multiple DUI offenders are more likely than the general population to suffer from comorbid psychiatric disorders in addition to a substance use disorder. Therefore, DUI treatment programs will need to include a comprehensive assessment of pathology and develop treatment plans that account for complex psychiatric profiles.
**The truncated CIDI assessed past-year and lifetime alcohol abuse and dependence, drug abuse and dependence, nicotine dependence, pathological gambling, major depression, mania, hypomania, dysthymia, generalized anxiety disorder, posttraumatic stress disorder, and conduct disorder. Authors added assessment for intermittent explosive disorder and attention-deficit hyperactivity disorder after 107 people had completed the CIDI.
—Leslie Bosworth
What do you think? Please use the comment link below to provide feedback on this article.
References
Kessler, R. C., Berglund, P., Demler, O., Jin, R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 593-602.
Lapham, S. C., Smith, E., C’de Baca, J., Chang, I., Skipper, B. J., Baum, G., et al. (2001). Prevalence of psychiatric disorders among persons convicted of driving while impaired. Archives of General Psychiatry, 58, 943-949.
Nelson, S. E., LaPlante, D. A., Peller, A. J., LaBrie, R. A., Caro, G., & Shaffer, H. J. (2007). Implementation of a computerized psychiatric assessment tool at a DUI treatment facility: A case example. Administration and Policy in Mental Health, 34, 489–493.
Shaffer, H. J., Nelson, S. E., LaPlante, D. A., LaBrie, R. A., & Albanese, M. (2007). The epidemiology of psychiatric disorders among repeat DUI offenders accepting a treatment-sentencing alternative option. Journal of Consulting and Clinical Psychology, 75(5), 795-803.