Past research has shown that people with gambling problems are at higher risk for comorbid disorders, particularly substance use disorders, than the rest of the population (see WAGER 10(12)), and that people with psychiatric disorders are at higher risk than others for gambling problems (Crockford & el-Guebaly, 1998; Shaffer, Hall, & Vander Bilt, 1999). However, this research is constrained by small samples and questionable measures. This week’s WAGER focuses on a recent study of pathological gambling among a large sample of psychiatric outpatients using a structured diagnostic interview.
Zimmerman, Chelminski, and Young (2006) measured psychiatric disorders among a sample of 1,709 people seeking treatment as outpatients at a psychiatric clinic in Rhode Island. Patients in the sample either carried health insurance or were able to afford services at the clinic. Sixty-two percent of participants were female and 87% were White. Interviewers assessed participants for all DSM Axis I disorders using the Structured Clinical Interview for DSM-IV (SCID) and a DSM-IV-based module for pathological gambling (PG). Table 1 displays the prevalence rates of the assessed disorders and their comorbidity with PG.
Table 1. Prevalence Rates of Psychiatric Disorders and Lifetime Comorbidity with Pathological Gambling Among Psychiatric Outpatients (N = 1,709). (Adapted from Zimmerman et al., 2006.)
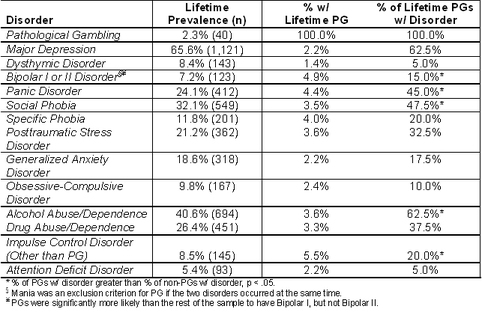
Zimmerman and colleagues found that 2.3% of the outpatient sample qualified for a lifetime diagnosis of PG. As Table 1 shows, PGs were more likely to have experienced bipolar disorder, social phobias, alcohol use disorders, and other impulse control disorders in their lifetime than the rest of the sample. PGs also experienced significantly more comorbidity during their lifetime than others in the sample, averaging 4.7 disorders. Twelve outpatients (0.7%) had current diagnoses of PG, but only three were seeking treatment through the clinic for PG.
These results indicate that lifetime PG rates are slightly elevated among psychiatric outpatients compared to rates found in the general population (i.e., 1.35%-1.85%: Shaffer et al., 1999), but that current rates are not (i.e., 0.7% compared to 0.90-1.38%: Shaffer et al., 1999). However, psychiatric outpatients who qualify for PG have significantly greater comorbidity than other outpatients.
There are a few limitations to the current study. The sample was located in a single geographic area. Because the clinic required insurance or out-of-pocket expense, the clinic population had higher SES than many people with psychiatric disorders. Both of these factors limit the generalizability of the findings. Finally, the clinic did not specialize in substance use disorders, which are known to be highly comorbid with PG; it is plausible that the comorbidity pattern would be different in a population with primary diagnoses of substance use disorders.
The findings from this study confirm the comorbidity of PG with other psychiatric disorders, but provide some evidence that PG is not particularly elevated among psychiatric samples compared to the rest of the population. Future research needs to begin to examine the temporal patterns of PG and other psychiatric disorders, identifying how much these disorders co-occur in time and whether certain disorders tend to precede or follow PG.
What do you think? Comments on this article can be addressed to Sarah Nelson.
References
Crockford, D. N., & el-Guebaly, N. (1998). Psychiatric comorbidity in pathological gambling: A critical review. Canadian Journal of Psychiatry, 43(1), 43-50.
Shaffer, H. J., Hall, M. N., & Vander Bilt, J. (1999). Estimating the prevalence of disordered gambling behavior in the United States and Canada: A research synthesis. American Journal of Public Health, 89(9), 1369-1376.
Zimmerman, M., Chelminski, I., & Young, D. (2006). Prevalence and diagnostic correlates of DSM-IV pathological gambling in psychatric outpatients. Journal of Gambling Studies, 22, 255-262.