David Comings’ research (1998), reviewed in WAGER 30, discussed the relatively higher prevalence of a particular genetic configuration in pathological gamblers. Similarly high incidences were found in subjects with disorders such as PTSD, alcoholism, and autism. Comings proposed the existence of a spectrum disorder which transcends discrete diagnostic categories to include a wide range of impulsive, compulsive, and addictive maladies. But the mere presence of a particular allele does not automatically produce addiction, just as the presence of clouds does not automatically lead to rain. The neural mechanisms at work are complex, and deserve attention.
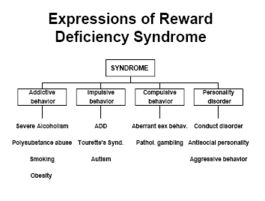
Blum, Cull, Braverman, and Comings (1996) describe in detail the neural system responsible for transmitting messages of reward and pleasure. They use as a starting point the work of James Olds (1954), who identified a part of the limbic system in rats that seemed to regulate reward. When presented with the opportunity to electrically stimulate this particular neural site by pressing a lever, the rat would do so as many as 5,000 times an hour. To maintain, the stimulation it would endure pain and forego other opportunities with the sole exception of sleep. Since then researchers have refined the idea of reward pathways and have identified several chemicals and parts of the human neuroanatomy that seem to play a part in the system (see table). Blum et al (1996) propose a “cascade” model of reward transmission, in which neurotransmitters engage in a chain reaction that spans several parts of the brain. The ultimate product of this cascade series is the release of dopamine, the neurotransmitter that has long been associated with reward and pleasure. In the case of an addicted individual, the chain reaction is partially dysfunctional, resulting in relatively lower levels of dopamine. Such a deficiency may cause the addict to experience cravings. Alcohol, cocaine, and nicotine all increase dopamine release, providing a temporary restoration of normal cascade function. That is, the substances serve as short-term boosters to a system that is reward-deficient. The cascade theory, however, does little to settle the age-old dispute between those who claim genetics as the etiology of addiction and those who point to environmental factors. Rather, the theory cites three separate phemomena as possible causes of reward deficiency syndrome, the name the authors give to the dysfunction of the limbic systems described above. Particular genetic variations, particularly of the D2 gene, seem to create neurobiological conditions that inhibit the cascade mechanism that should result in proper dopamine release. Long-term stress can have a similar effect, as can the extended abuse of a substance itself.
Several pharmaceutical approaches are being studied with the hope of restoring normal function to the reward-deficient limbic system. So far, the research among a cohort of alcoholics seems promising.3 The resemblance between pathological gambling and other addictions has long been noted, but such a resemblance does not necessarily mean that the syndrome is involved in the former. Further research must be conducted to determine whether reward-deficiency syndrome and its potential pharmaceutical antidote apply to disordered gambling.
This public education project is funded, in part, by The Andrews Foundation and the National Center for Responsible Gaming.
This fax may be copied without permission. Please cite The WAGER as the source.
For more information contact the Massachusetts Council on Compulsive Gambling, 190 High Street, Suite 6, Boston, MA 02110, U.S.




Martin Buuri Kaburia June 30, 2017
Wonderful study