Emergency rooms (ER) are an essential part of the healthcare system, specializing in caring for patients who need immediate assistance. Within the past ten years, ERs have been increasingly used to treat substance use and mental health concerns, both of which are risk factors for intentional and/or unintentional self harm or suicide and other health-related concerns, such as cancer and poor quality of life. This week, STASH reviews a study by Silas Wang and colleagues that identified types of substance use and mental health conditions associated with ER visits.
What was the research question?
What types of substance use and mental health conditions do individuals most frequently seek treatment for in ERs?
What did the researchers do?
The researchers used data collected in 2020 from the U.S. National Surveys on Drug Use and Health (NSDUH) dataset to analyze past-year ER visits, past-year substance use1 and dependence, and past-year mental health conditions2 among a sample of 26,325 participants aged 18 and older. They also gathered background information on participants, such as gender, age, race/ethnicity, income, and level of educational attainment. The researchers used a cluster analysis to divide strongly correlated variables into groups and multivariate logistic regression to estimate the odds ratio for the association between substance use/mental health variables and ER visits.
What did they find?
Of the sample, 21.9% visited the ER in the past year, with females (23.8%) being more likely than males (19.8%). Participants aged 65+ were more likely to visit the ER than those aged 18-25. Compared to non-Hispanic Whites, Black participants were more likely, and Asian participants were less likely, to have had an ER visit. Those with relatively low income and low educational attainment also had greater risk for ER visits. Through the cluster analysis, Wang and colleagues found that people most frequently visited the ER for opioid-related concerns compared to any other substance use/mental health concern. The multivariate logistic regression analysis identified 15 substance use and mental health variables that were associated with past-year ER visits (see Figure). Surprisingly, heavy alcohol use in the past month and misuse of general pain relievers were associated with a decreased likelihood of visiting the ER. Other variables like nicotine dependence, having suicidal plans in the past year, and oxycodone use were associated with increased risk (see Figure).
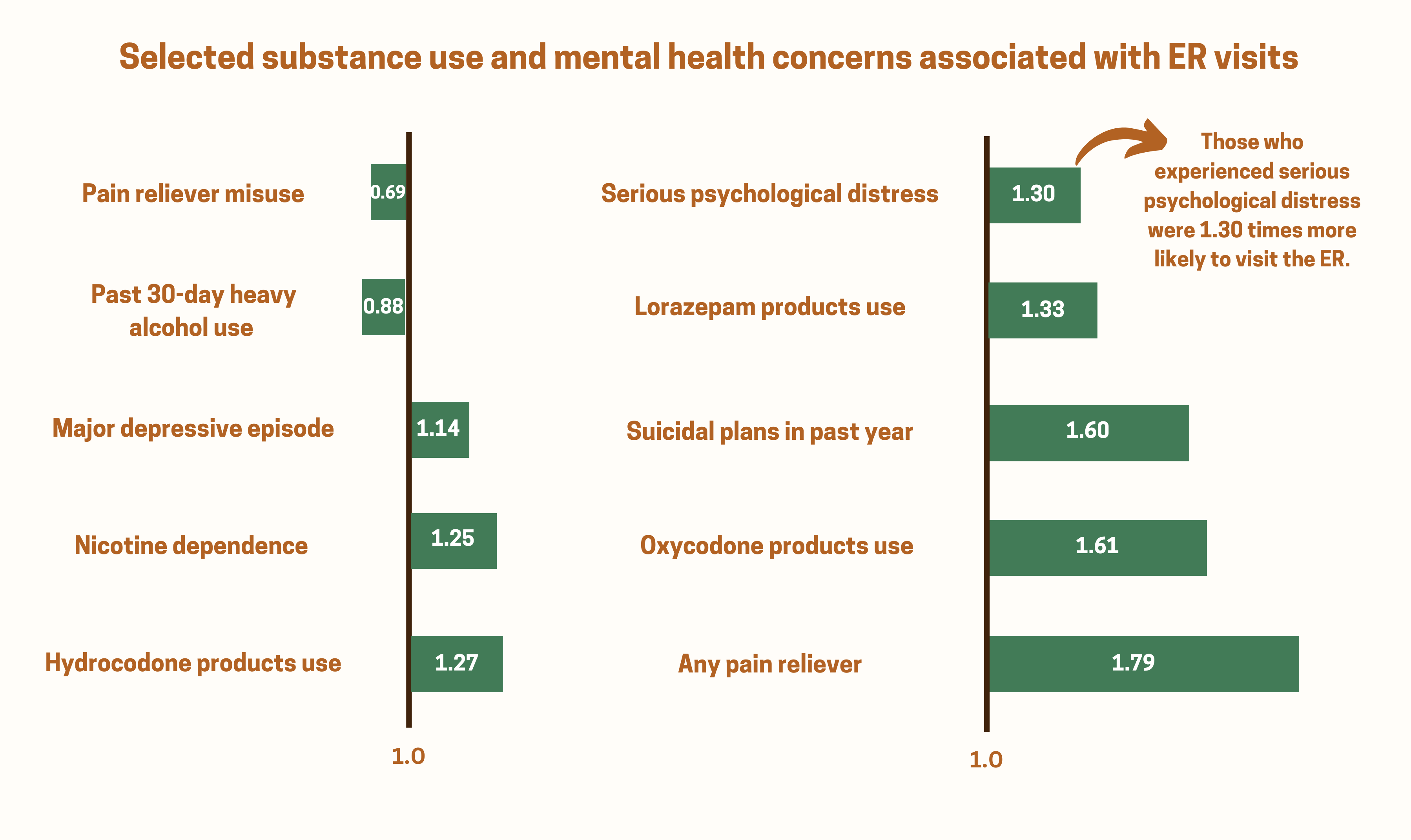
Figure. Odds ratio for the association between substance use/mental health concerns and ER visits. An odds ratio <1 indicates a decreased likelihood of ER visits. An odds ratio > 1 indicates an increased likelihood of ER visits. Click image to enlarge.
Why do these findings matter?
Given that drug overdoses continued to escalate in 2020, it is unsurprising that opioid use emerged as the most common reason for ER visits, compared to the other identified substance use and mental health variables. However, it is important to note that patients presenting to the ER after a drug overdose likely experience other substance use and mental health conditions, because these conditions often co-occur and present the same barriers to primary care and outpatient treatment. Additionally, these barriers disproportionately impact racial and ethnic minority groups. Implementing culturally appropriate, evidence-based treatment interventions could address some of these barriers. For example, efforts like the How Right Now (Qué Hacer Ahora) campaign uses a strengths-based perspective to promote mental health and resiliency among adults impacted by the COVID-19 pandemic through the use of culturally specific resources.
Every study has limitations. What are the limitations in this study?
The 2020 NSDUH dataset is composed of survey responses during the start of the COVID-19 pandemic – a time of increased substance use and mental health concerns – which could have skewed results. Additionally, the survey responses were self-reported and subject to social desirability bias. Lastly, the NSDUH data was cross-sectional which meant that we could not determine causality between substance use/mental health conditions and ER visits. Future research could focus on longitudinal studies to better analyze these associations.
For more information:
If you are worried that you or someone you know is experiencing addiction, the SAMHSA National Helpline is a free treatment and information service available 24/7. For more details about addiction, visit our Addiction Resources page.
— Nakita Sconsoni, MSW
________________
1. Past-year substance use variables include illicit drug use, nonmedical prescription drug use, and alcohol/tobacco use.
2. Past-year mental health variables include depression, psychological distress, and suicidal behavior.




