Many people with Opioid Use Disorder (OUD) experience other psychiatric disorders, such as depression and anxiety, which are painful and can exacerbate addiction. Their psychiatric symptoms often improve when they start taking medication for OUD (e.g., buprenorphine, methadone), but in order to receive that medication they are typically required to attend psychosocial counseling. This week, STASH reviews a study by Joanna Streck and colleagues that investigated whether patients experience improvement in psychiatric symptoms with buprenorphine in the absence of counseling.
What was the research question?
Do patients experience improvement in psychiatric symptoms while they are receiving buprenorphine but on a waitlist for counseling?
What did the researchers do?
The researchers studied fifty people who were on a waitlist for comprehensive OUD treatment (i.e., medication plus counseling). While they were on the waitlist for comprehensive treatment, half of the people started receiving buprenorphine alone and half got no treatment. They were randomly assigned to these groups. Participants completed assessments at baseline, then at 4, 8, and 12 weeks afterwards. During these assessments, participants completed the Beck Anxiety Inventory (BAI), the Beck Depression Inventory-II (BDI-II), the Brief Symptom Inventory (BSI), and the Addiction Severity Index (ASI). The researchers then examined the changes between the two groups on these measures across the 12-week study period.
What did they find?
Participants receiving buprenorphine experienced statistically significant decreases in anxiety, depression, and general psychiatric distress (as measured by both the BSI and ASI) after 4 weeks. These improvements lasted throughout the 12-week study. In comparison, participants in the no-treatment group did not experience any statistically significant decreases on any of these psychiatric assessments.
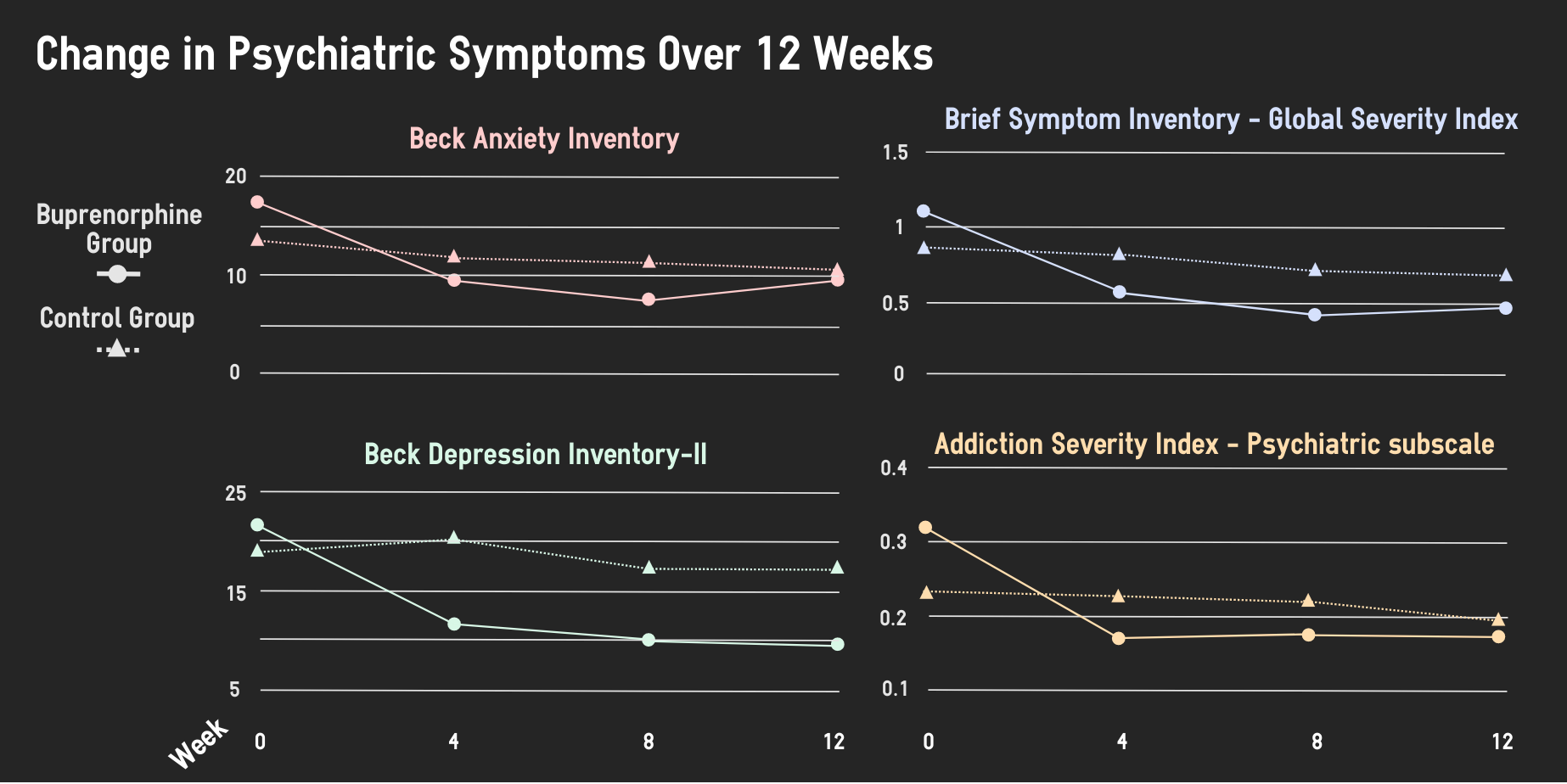
Figure. The graphs show the mean scores on each assessment for the buprenorphine group and waitlist control group across the study period. Adapted from Streck et al., 2018. Click image to enlarge.
Why do these findings matter?
Previous studies of OUD treatment have often combined medication and counseling, making it difficult to tell what aspect of treatment was responsible for the improvement in psychiatric symptoms. This study is among the first to show that these improvements might be attributable to medication (in this case, buprenorphine) itself. This set of findings calls into question the typical requirement that patients attend psychosocial counseling in order to receive medication for OUD. Of course, one size does not fit all, and some patients might experience real benefit from combining medication with counseling.
Every study has limitations. What are the limitations in this study?
This study only had fifty participants; replicating this experiment with a larger group of participants will reduce the margin of error of the results. Participants receiving buprenorphine not only knew they were receiving medication; they also received nightly phone calls to monitor their symptoms and random call-backs to visit the clinic roughly every two weeks. It is possible that their psychiatric symptom improvements at least partly resulted from a placebo effect or a sense of support from the phone calls and extra clinic visits.
For more information:
Are you worried about your own or a loved one’s addiction or mental health issues? The National Helpline is a free treatment and information services available 24/7. Our Addiction Resources page has free, anonymous resources for people concerned about substance use or other expressions of addiction.
— Rhiannon Chou Wiley
What do you think? Please use the comment link below to provide feedback on this article.