Since 2001, the U.S. government has deployed more than 1.6 million military personnel to Afghanistan or Iraq (Tanielian, et al. 2008). Among
veterans returning from these conflicts, doctors have observed nearly 200,000 cases of mild-traumatic brain injury (i.e., TBI; Fischer, 2013). Symptoms of mild-TBI include being confused/disoriented or experiencing memory loss for less than 24 hours, losing consciousness for up to thirty minutes, and normal medical imaging results (Fischer, 2013). Left untreated, TBI and other invisible wounds of war can lead to substance use disorders and a variety of psychiatric comorbid disorders (Tanielian, 2008). This week’s DRAM reviews an article that assessed the risk for addiction following a mild-TBI among active-duty military personnel (Miller et al., 2013).
Methods
- Researchers conducted a historical prospective study of nearly 50,000 US Air Force service members drawn from a sample of 500,000 who were on active duty for at least half a year during the years 2001 and 2008.
- The sample was made up of mostly white males with less than a high school diploma who have never been married.
- Researchers identified both mild-TBI and addiction-related disorders by looking for the corresponding diagnostic codes in each airman’s medical records. They classified addiction-related disorders as having occurred at either 1-30 days, 31-179 days, or at least 180 days post-injury.
- Researchers excluded airmen with a history of mild-TBI, other head injuries, or addiction-related disorder within 2 years prior to inclusion in the study.
- The study sample included a cohort of 5,065 airmen who experienced a mild-TBI during the study period and a comparison cohort of 44,733 airmen who experienced a different outpatient injury, but no TBI, during the study period.
- Researchers conducted Cox proportional hazard regression analyses (a form of survival analysis), while controlling for confounders, to determine the risk of substance abuse or dependence among those suffering from mild-TBI compared to the rest of the sample.
Results
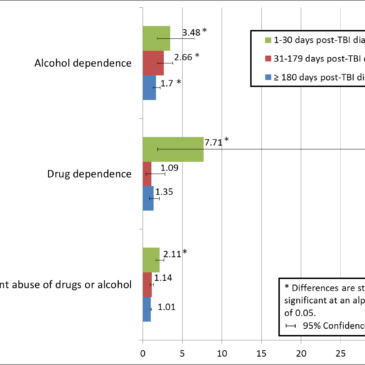
- Compared to other injured military personnel, those with mild-TBI were at increased risk for certain addiction-related disorders (see Figure).
- Alcohol dependence was significantly elevated at all three time points post-diagnosis for personnel with mild-TBI.
- The risk for alcohol dependence was most elevated for these personnel at 1-30 days post-diagnosis with consistent decreases at each subsequent time interval.
- For drug dependence and nondependent abuse of drugs or alcohol, the risk for mild-TBI personnel was only elevated for the period of observation immediately following the mild-TBI diagnosis.

Figure. Adjusted hazard ratios for alcohol and drug abuse and dependence among active-duty US airmen with mild-TBI compared to other-injured airmen (adapted from Miller et al., 2013). Click image to enlarge.
Limitations
- Some airmen who truly had mild-TBI might have been misclassified as not having had mild-TBI. This could happen as a result of diagnostic errors or airmen’s reluctance to seek medical help. This misclassification would lead to an underestimate of risk for substance use disorders.
- Along the same lines, some airmen with addiction-related disorders might have been misclassified as not having had addiction-related disorders, particularly if those disorders go unreported and untreated. This misclassification of the outcome would lead to an underestimate of the risk for substance use disorders.
Conclusions
Military personnel who suffer mild traumatic brain injuries are at increased risk for substance abuse and dependence for a variety of substances, mainly in the period immediately following their injury. In particular, alcohol dependence might be a long lasting effect of mild-TBI. It’s possible airmen are abusing substances to cope with the symptoms of mild-TBI or because their injury has made them more susceptible to addiction. Substance misuse might inhibit the healing process and lead to long-term health problems, which could then exacerbate substance use problems. Screening for substance use and abuse following a mild-TBI should be considered for all military personnel at risk for TBI.
– John Kleschinsky
What do you think? Please use the comment link below to provide feedback on this article.
References
Fischer, H. (2013). U.S. military casualty statistics: Operation new dawn, operation iraqi freedom, and operation enduring freedom (RS22452). Washington DC: Congressional Research Service.
Miller, S.C., Baktash, S.H., Webb, T.S., Whitehead, C.R., Maynard, C., Wells, T.S., Otte, C.N., Gore, R.K. (2013). Risk for Addiction-Related Disorders Following Mild Traumatic Brain Injury in a Large Cohort of Active-Duty U.S. Airmen. American Journal of Pschiatry, EPub ahead of print 2013 Feb 22.
Tanielian T., Jaycox L.H., Schell T.R., Marshall G.N., Burnam M.A., Eibner C., Karney B.R., Meredith L.S., Ringel J.S., Vaiana M.E. (2008). Invisible wounds of war: summary and recommendations for addressing psychological and cognitive injuries. Santa Monica, Calif, Rand
Corp. http://rand.org/pubs/monographs/2008/RAND_MG720.1.pdf