People with gambling-related problems also are likely to qualify for other psychiatric disorders (McIntyre et al., 2007; Shaffer et al., 2007). Understanding the temporal sequence of PG and comorbid disorders can provide information about how PG relates to other disorders and suggests causal links. Unfortunately, there is little research that clarifies how the onset of PG relates temporally to the onset of other disorders. This week’s WAGER reviews a large epidemiological study by Kessler, Hwang, LaBrie, Petukhova, Sampson, Winters & Shaffer (2008), which investigated comorbid disorders among people with PG. In addition, this study examined the temporal onset of PG and the onset of other disorders.
The National Comorbidity Survey Replication (NSC-R), a nationally representative sample of 9,282 English speaking adults (Kessler & Merikangas, 2004), used the Composite International Diagnostic Interview (CIDI; Kessler & Ustun, 2004) to assess DSM-IV criteria (American Psychiatric Association, 1994) for Axis I disorders, and age of onset (AOO; i.e., the age at which people first reported the first symptom of a given disorder) for those with disorders.
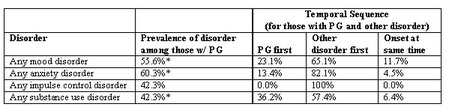
Table 1. Lifetime psychiatric comorbidity among participants with lifetime PG (adapted from Kessler et al., 2008)
* Prevalence significantly greater among PGs compared to the rest of the sample (p < .05).
Note: Any mood disorder = major depressive disorder or dysthymia and bipolar disorder. Any anxiety disorder = phobias, generalized anxiety, panic, and post-traumatic stress disorder. Any impulse control disorder = oppositional-defiant, conduct, attention deficit hyper activity, and intermittent explosive disorders. Any substance use disorder = alcohol or drug abuse, dependence, and nicotine dependence.
The lifetime prevalence of pathological gambling (PG) within the sample was 0.6%. Almost all participants who had lifetime PG also had another lifetime disorder (96.3%) and 64.3% suffered from three or more disorders. Table 1 shows that mood disorders, anxiety disorders, and substance use disorders were significantly elevated among participants with PG, and that other disorders were more likely to precede PG than to occur afterward or begin at the same time. In fact, 74.3% of participants with PG and another disorder experienced the other disorder before PG.
These results provide important information about the temporal relationships among disorders. However, this study cannot conclusively determine whether any disorder caused PG, or PG caused another disorder. Furthermore, the data in this study derived from retrospective self-report; consequently, AOO might not be accurate because of recall errors. However, the results suggest that PG rarely exists alone. This study adds important new data about typical pattern of onset. The study also illuminates the need for mental health and medical professionals to assess PG along with the variety of other disorders with which it is often comorbid.
What do you think? Comments can be addressed to Leslie Bosworth.
References
American Psychiatric Association. (1994). DSM-IV: Diagnostic and statistical manual of mental disorders (Fourth ed.). Washington, D.C.: American Psychiatric Association.
Kessler, R. C., Hwang, I., LaBrie, R., Petukhova, M., Sampson, N. A., Winters, K. C., et al. (in press). DSM-IV pathological gambling in the National Comorbidity Survey Replication. Psychological Medicine [preprint available]
Kessler, R. C., & Merikangas, K. R. (2004). The National Comorbidity Survey Replication (NCS-R): Background and aims. International Journal of Methods in Psychiatric Research, 13(2), 60-68.
Kessler, R. C., & Ustun, T. B. (2004). The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). International Journal of Methods in Psychiatric Research, 13(2), 93-121.
McIntyre, R. S., McElroy, S. L., Konarski, J. Z., Soczynska, J. K., Wilkins, K., & Kennedy, S. H. (2007). Problem gambling in bipolar disorder: Results from the Canadian Community Health Survey. Journal of Affective Disorders, 102(1), 27-34.
Shaffer, H. J., Nelson, S. E., LaPlante, D. A., LaBrie, R. A., Albanese, M., & Caro, G. (2007). The epidemiology of psychiatric disorders among repeat DUI offenders accepting a treatment sentencing option Journal of Consulting and Clinical Psychology, 75(5), 795-804.




Lynne O April 28, 2016
The article in this month’s wager on problem gambling and other psychiatric comorbidity is interesting.
Is problem gambling perhaps a good indicator of an underlying psychiatric disorder?
Could pathological gambling (PG) be like having a high temperature, i.e., not a cause but a side effect?
Could problem gambling be a side effect which is readily recognised and could therefore be used as an early warning device for detecting psychiatric disorders?
Cheers,
The BASIS Staff April 28, 2016
Dear Ms. O:
Thank you for your comment about the WAGER volume 13(2) – Chickens, Eggs, and Psychiatric Comorbidity among PGs.
Based on the current evidence, we think that pathological gambling is a psychiatric disorder, and it seems to be a proxy for the presence of additional psychiatric disorders, among other things. In addition, PG might indicate that those with this diagnosis qualified for other disorders during their lifetime, but not currently.
Comparing PG to a high body temperature (fever) is an interesting analogy that we also have used. The National Comorbidity Study Replication (NCS-R) reveals the sequence of disorders, and shows that other problems typically precede and potentially stimulate gambling problems. The NCS-R, however, is designed so that it can only measure associations. Although we can determine that there is a relationship between PG and other disorders, we only can infer the nature of this relationship and the factors that mediate the association. This means designating psychiatric disorders as a cause for PG or PG as a side effect of a psychiatric disorder is beyond the scope of the NCS-R. This is a subject area that needs and deserves more prospective research.
PG could be a warning device for detecting psychiatric disorders, much as smoking tobacco in the United States is now. The social context of these phenomena is important to consider. Finally, prevention programs look for opportunities to identify the “proxy” that reliably predicts other problems as early in the sequence of events as possible and then tries to change them. If we can make life worth living, fewer people need to attenuate or escape their lives. Of course we still need to permit that some people – the minority – have problems with gambling or other objects of addiction without any preceding psychopathology. However, this group is few in number.
Faculty at the Division on Addiction have promulgated a Syndrome Model of Addiction. Your questions allude to some parts of this model. A complete description of the model might help connect your questions into a more comprehensive understanding of addiction, including pathological gambling as one expression of addiction, and how various expressions of addiction can relate to psychiatric disorders. You can find original syndrome model paper in the following publication:
Shaffer, H. J., LaPlante, D. A., LaBrie, R. A., Kidman, R. C., Donato, A. N., & Stanton, M. V. (2004). Toward a syndrome model of addiction: Multiple expressions, common etiology. Harvard Review of Psychiatry, 12, 367-374.
Some BASIS articles briefly describe and discuss the Syndrome Model. Links to those articles are below:
http://www.basisonline.org/2007/05/addiction_the_h.html
http://www.basisonline.org/2007/02/the_dram_vol_32.html
Thank you again for your questions and feedback.