STASH 10(14): Perceived discrimination as a risk factor for substance use disorders
Recent events have brought perceived racial discrimination, particularly in the context of police interactions, to the forefront of the country’s consciousness. Researchers have previously explored the link between experiences of discrimination and stress-sensitive mental health disorders among racial and ethnic minorities (Hunte & Barry, 2012). However, there are many unanswered questions. For example, do certain types of discrimination increase the risk for specific disorders, such as drug abuse and depression? Does more frequent perceived discrimination lead to more negative outcomes? This week, we review a study that examined the link between perceived discrimination and mental health/substance use disorders among American racial minorities (Clark et al, 2015).
Methods
- The researchers used data from the National Survey of American Life (NSAL; Jackson et al., 2004), looking at a subsample of 4,462 adults of African-American and/or Caribbean Black background.
- They clustered their sample into four groups based on self-reported frequency and type of perceived racial discrimination in everyday life, as measured by the Everyday Discrimination Scale (EDS; Williams, Yu, Jackson, & Anderson, 1997). The EDS includes nine questions about experiences of discrimination, ranging from experiences of relatively minor disrespect and condescension (e.g., “How often do you receive poorer service than others at restaurants or stores?”) to graver instances of hostile or character-based discrimination (“How often are you harassed or threatened?”).
- The Low Discrimination group reported very low levels of perceived discrimination. They represented 17% of the sample.
- The Disrespect and Condescension group reported recurrent experiences of disrespectful/condescending discrimination only. They represented 17% of the sample.
- The General Discrimination group reported recurrent experiences of both disrespectful/condescending and hostile/character-based discrimination. They represented 51% of the sample.
- The Chronic Discrimination group reported frequent experiences of disrespectful/condescending discrimination and recurrent experiences of hostile/character-based discrimination. They represented 15% of the sample.
- The NSAL also assessed a range of mental disorders using a modified version of the WHO-CIDI (Kessler & Üstün, 2004). For this study, the researchers classified respondents according to whether they ever, during their lifetimes, met criteria for major depressive disorder, generalized anxiety disorder, alcohol use disorder,1 and illicit drug use disorder.2
- The researchers predicted that people who reported experiencing more severe discrimination would be more likely to meet criteria for mood and drug use disorders.
Results
- The researchers found that perceived discrimination was associated with mood, anxiety, and substance use disorders.
- More specifically, compared to those in the Low Discrimination group,
- Participants in the General Discrimination and Chronic Discrimination groups were more likely to meet criteria for major depression.
- Participants in the Chronic Discrimination group were more likely to meet criteria for anxiety disorder.
- Participants in the Disrespect and Condescension, General Discrimination, and Chronic Discrimination groups were all more likely to meet criteria for alcohol use disorders. Participants in the General Discrimination and Chronic Discrimination groups were more likely to meet criteria for illicit drug use disorders. (See Figure 1.)
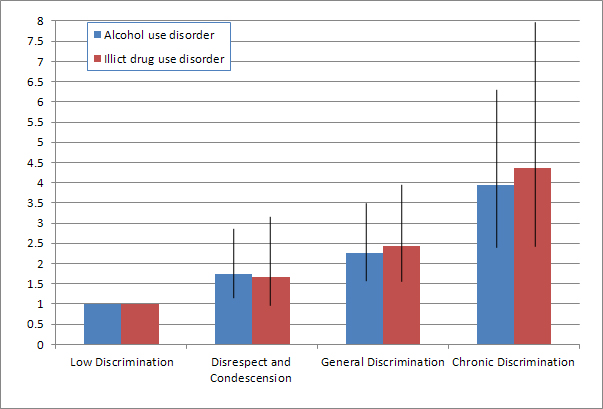
Figure. Risk ratios and Confidence Intervals of having a lifetime alcohol or illicit drug use disorder based on frequency and type of perceived discrimination (adapted from Clark et al., 2015). Note: The Low Discrimination group was used as reference group for risk ratio estimates. Click image to enlarge.
Limitations
- Self-reported data is always subject to memory errors and impression management biases.
- The study could not look at the development of mood or drug use disorders over time, and so it might have missed some of the complexity of the relationship between onset of substance use, depression, and discrimination. Researchers only looked at self-reported lifetime prevalence of symptoms.
- The researchers did not specify that they asked participants if they attributed their perceived discrimination explicitly to their race or ethnicity, or to some other aspect of their physical appearance such as gender, age or weight.
Conclusions
The results of this study indicate a strong link between perceived discrimination—particularly that of a hostile or character-based nature— and risk for substance use and mood disorders. Most strikingly, people who reported chronic discrimination were over four times more likely to abuse or be dependent on illicit drugs. It is also noteworthy that in this general population study, 51% of the sample reported recurrent or even frequent experiences of disrespectful/condescending and hostile/character-based discrimination.
Due to the cross-sectional nature of the study, the precise link between perceived discrimination and mental health is unclear; there are several plausible pathways. People who experience more frequent discrimination, especially of a hostile and threatening nature, might be more likely to turn to drugs to deal with stress. It is also possible that people with mood and drug use disorders are more likely to perceive discrimination and threats coming their way—perhaps because they adopt a ruminative style, causing them to dwell on negative experiences and remember specific instances of discrimination. Future studies could gather longitudinal data starting in adolescence to determine the complex interaction between discrimination and onset of substance use and mood disorders.
– Kat Belkin
What do you think? Please use the comment link below to provide feedback on this article.
References
Clark, T.T., Salas-Wright, C.P., Vaughan, M.G., Whitfield, K.E. (2015). Everyday discrimination and mood and substance use disorders: A latent profile analysis with African Americans and Caribbean Blacks. Addictive Behaviors, 40, 119-125
Hunte, H. E., & Barry, A. E. (2012). Perceived discrimination and DSM-IV-based alcohol and illicit drug use disorders. American Journal of Public Health, 102(12), e111–e117.
Jackson, J. S., Torres, M., Caldwell, C. H., Neighbors, H. W., Nesse, R. M., Taylor, R. J., et al. (2004). The National Survey of American Life: A study of racial, ethnic and cultural influences on mental disorders and mental health. International Journal of Methods in Psychiatric Research, 13(4), 196–207
Kessler, R. C., & Üstün, T. B. (2004). The World Mental Health (WMH) Survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). International Journal of Methods in Psychiatric Research, 13(2), 93- 121.
Williams, D. R., Yu, Y., Jackson, J. S., & Anderson, N.B. (1997). Racial differences in physical and mental health socio-economic status, stress and discrimination. Journal of Health Psychology, 2, 335–351.
________________
[1] Defined as abuse or dependence.
[2] Also defined as abuse or dependence.