ASHES, Vol. 8(2): Two meds are better than one? Examining the success of combination therapies for smoking cessation
Mounting evidence suggests that combinations of nicotine replacement therapies (NRTs) are more effective at improving cessation rates than single therapies ((Piper et al., 2009; Smith et al., 2009) Research on single therapies suggest that these therapies work in part by affecting factors such as craving and withdrawal (McCarthy et al., 2008; Piper et al., 2008). This week’s ASHES reviews a study of potential mediators for combination pharmacotherapies’ superior smoking cessation outcomes compared to monotherapies (Bolt, Piper, Theobald, & Baker, 2012).
Methods
- 1,504 current smokers (41.8% male, 83.9% White) who wished to quit smoking were randomized to one of six cessation pharmacotherapy conditions: Placebo (matched to the other conditions); Nicotine patch; Nicotine lozenge; Bupropion; Nicotine patch + nicotine lozenge; and, Bupropion + nicotine lozenge.
- Researchers provided all medications for 8-12 weeks post-quit. In addition, each patient received six counseling sessions.Measures
- Participants completed questionnaires at baseline that assessed demographic information, smoking history and tobacco dependence.
- The researchers assessed abstinence by recording abstinence at 8 weeks post-quit (i.e., carbon monoxide levels at < 10ppm).
- The researchers used ecological momentary assessment (EMA) to examine craving, withdrawal, negative affect, positive affect, and expectation of smoking reward four times a day. Participants reported via EMA for one week pre-quit and two weeks post-quit.
- These potential mediators were divided among two distinct parameters:
- “Jump” or how each of the mediating variables changed on the quit day
- “Slope” or the average daily rate of change in the mediating variables over two weeks post-quit
Results
- Treatment effects on 8-week post-quit abstinence rates for monotherapies and combination therapies differed significantly from each other. Abstinence rates were 45% and 54% respectively. Placebo post-quit abstinence rates were statistically significantly lower than each, at 33%.
- Univariate analyses suggested that craving, negative affect, and expectations mediated the relationship between replacement therapy and abstinence, but withdrawal and positive affect did not.
- Across mediators, the more substantial effects of treatment consistently occurred with respect to the jump rather than the post-quit slope
- Subsequent multivariate modeling determined that the effects associated with negative affect and expectations became non-significant when tested in a model with craving (see Table 2).
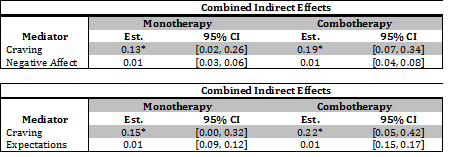
Figure. Results From Multivariate Mediation Analysis: Craving, Negative Affect, and Smoking Expectations (Bolt, et al., 2012 Click image to enlarge.
Limitations
- The number of potential mediators was limited. Additional unmeasured variables could have played important roles.
- The mediators required self-reported experiences. It is possible that craving and the other mediating variables could have different value for different smokers, due to varying interpretations of those subjective experiences.
Discussion
This study tested combination pharmacotherapies, compared them to monotherapies, and used meditational analysis to compare the contributions of the potential mediators. Findings suggest that the superiority of combination therapy might relate to its ability to suppress early craving experiences. More specifically, jump in craving seen on the quit day proved to be more important than the trajectory of craving over the 2-week post-quit period, and other potential mediators. This is in line with other recent research that implicates craving in early-stage quit attempts as a critical determinant of long-term outcomes in abstinence (McCarthy, et al., 2008; Piper, et al., 2008). In the future, public health efforts could focus on monitoring people who report more severe cravings upon quitting and finding ways to target them with combination therapy.
–Kat Belkin
References
Bolt, D. M., Piper, M. E., Theobald, W. E., & Baker, T. B. (2012). Why two smoking cessation agents work better than one: Role of craving suppression. Journal of Consulting and Clinical Psychology, 80(1), 54-65.
McCarthy, D. E., Piasecki, T. M., Lawrence, D. L., Jorenby, D. E., Shiffman, S., & Baker, T. B. (2008). Psychological mediators of bupropion sustained-release treatment for smoking cessation. Addiction, 103, 1521-1533.
Piper, M. E., Federmen, E. B., McCarthy, D. E., Bolt, D. M., Smith, S. S., Fiore, M. C., et al. (2008). Using mediational models to explore the nature of tobacco motivation and tobacco treatment effects. Journal of Abnormal Psychology, 117, 94-105.
Piper, M. E., Smith, S. S., Schlam, T. R., Fiore, M. C., Jorenby, D. E., Fraser, D., et al. (2009). A randomized placebo-controlled clinical trial of 5 smoking cessation pharmacotherapies. Archives of General Psychiatry, 66, 1253-1262.
Smith, S. S., McCarthy, D. E., Japuntich, S. J., Christiansen, B., Piper, M. E., Jorenby, D. E., et al. (2009). Comparative effectiveness of 5 smoking cessation pharmacotherapies in primary care clinics. Archives of Internal Medicine, 169(2148-2155).
What do you think? Please use the comment link below to provide feedback on this article.