STASH, Vol. 7(6) – Primary care treatment for people with opiate addiction: Stronger support for a team effort
Fewer than 25% of individuals who are opioid dependent receive addiction treatment (SAMHSA, 2007). Within general medical practices, buprenorphine is a promising tool for the treatment of opioid dependence; this strategy is commonly referred to as office-based opioid treatment (OBOT). However, many physicians cite insufficient nursing support as a barrier to their use of OBOT (Walley et al., 2008). Boston Medical Center has instituted a collaborative care OBOT program that emphasizes collaboration among nurses, physicians, and pharmacists. In this week’s STASH, we review a new study that describes the effectiveness of this program and explores potential patient-level moderators of treatment success (Alford et al., 2011).
Methods
- Four hundred eight patients with opioid addiction took part in the program (M age = 39 years; SD = 11; 66.5% White, 16.5% Black, and 15.4% Hispanic; 66.0% Male). Researchers excluded 26 patients who left treatment because of preexisting legal or medical conditions or a need to re-locate from the analyses.
- The collaborative care OBOT program included a full-time nurse program director, nurse care managers (NCMs), a program coordinator, and generalist physicians with part-time clinical practices. NCMs’ clinical responsibilities included assessment, patient education, development treatment plans, overseeing medication management, monitoring treatment adherence, and communicating with other providers. Physicians examined patients, prescribed buprenorphine, and provided follow-up as needed.
- The treatment model included 3 stages:
- Assessment: The nurse program director screened patients and triaged them to intake appointments. At intake, NCMs and physicians jointly administered a thorough medical evaluation and developed a treatment plan.
- Induction and Stabilization: Physicians prescribed buprenorphine and NCMs monitored induction, which occurred on-site on Day 1, and dose stabilization, which occurred at home on Days 2-7. NCMs assessed for withdrawal and adverse effects.
- Maintenance: Staff provided ongoing monitoring at follow-up appointments at least weekly for the first 4 to 6 weeks followed by visits every 2 to 4 weeks if adherent, gradually tapering out to once a month and then once every 3 months. NCMs conducted scheduled and random callback urine drug tests at least once every 3 months, and encouraged patients to attend self-help groups and mandatory weekly addiction counseling.
- The researchers defined treatment adherence as 4 consecutive urine drug tests with negative results for illicit drugs; study participants also needed to evidence positive results for buprenorphine, and attend at least 3 of 4 counseling sessions per month.
- To fulfill the criteria for successful treatment, patients had to meet three conditions:retention at 12 months with a consistent pattern of treatment adherence
- buprenorphine dosage taper after 6 months of treatment adherence
- absence of illicit opiate use for at least 6 months
Results
- At 1 year, 196 of 382 patients (51.3%) underwent successful treatment, 162 patients (42.4%) showed an unsuccessful outcome, and 24 (6.3%) transferred to methadone maintenance treatment for more structured care or for full opioid agonist therapy.
- Urinalysis indicated a 4.7% opioid positive test rate for patients who were still in the OBOT program at 12 months.
- As Figure 1 illustrates, moderators of treatment success include age, race, employment, and illicit buprenorphine use. Patients who were older, employed, and self-maintained with illicit buprenorphine had significantly higher odds of treatment success (all p’s < 0.05). Those of African American or Hispanic/Latino race had significantly lower odds of treatment success (p’s < 0.05).
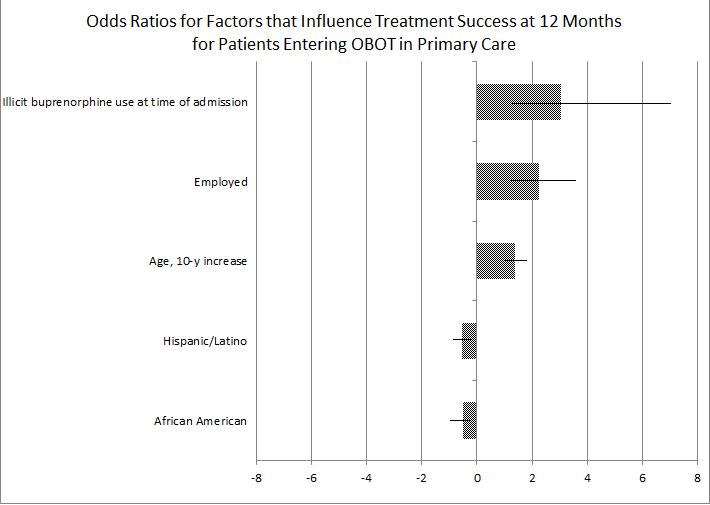
Figure. Odds Ratios for Factors that Influence Treatment Success at 12 Months for Patients Entering OBOT in Primary Care. Click image to enlarge.
Limitations
- This study did not have a control group. This makes it impossible to directly compare the effectiveness of the program to other traditional methods of care.
- Follow-up information was not available after patient departure for the program. A broader scope of outcomes is needed to assess the success of the OBOT program.
Discussion
This study shows some support for OBOT within a collaborative care model. The results compare favorably to those of similar programs that treat opioid addiction. Gerra et al. (2006) found a 43.8% retention rate at 12 months for heroin users accepting buprenorphine treatment in an outpatient setting, and Pinto et al. (2010) report a 50% retention rate at 6 months for a buprenorphine treatment program with less clinical support. Methadone treatment consistently has evidenced a higher retention rate than buprenorphine treatment, but has shown no difference in suppression of illicit opioid use for those who remain in treatment (Mattick et al., 2008; Fischer et al., 1999). The high level of clinical support and role sharing in the collaborative care model might account for some treatment success, but a 51.3% retention rate is difficult to applaud – treatment can do better.
The finding that self-maintaining with illicit buprenorphine at admission predicted later success is interesting. Schuman-Olivier et al. (2010) found that individuals who are dependent on opioids often illicitly use buprenorphine to manage pain and withdrawal rather than to get high. Similarly, Alford et al. speculate that those who used buprenorphine illicitly at pre-admission are highly motivated to find a safe and affordable source of buprenorphine for treatment of withdrawal symptoms. Further study is needed to better understand the ways that race, age, and employment status predict success in OBOT.
-Kat Belkin
What do you think? Please use the comment link below to provide feedback on this article.
References
Alford, D. P., LaBelle, C.T., Kretsch, N., Bergeron, A., Winter, M., Botticelli, M., Samet, J.H. (2011). “Collaborative Care of Opioid-Addicted Patients in Primary Care Using Buprenorphine: Five-Year Experience.” Archives of Internal Medicine 171(5): 425-431.
Fischer, G., Gombas, W., Eder, H., Jagsch, R., Peternell, A., Stühlinger, G., Pezawas, L., Aschauer, H.N., Kasper, S. (1999). “Buprenorphine versus methadone maintenance for the treatment of opioid dependence.” Addiction 94(9): 1337-1347.
Gerra, G., Leonardi, C., D’Amore, A., Strepparola, G., Fagetti, R., Assi, C., Zaimovic, A., Lucchini, A. (2006). “Buprenorphine treatment outcome in dually diagnosed heroin dependent patients: A retrospective study.” Progress in Neuropsychopharmacology and Biological Psychiatry 30(2): 265-272.
Mattick, R. P., Kimber, J., Breen, C., Davoli, M. (2008). “Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence.” Cochrane Database of Systematic Reviews (2).
Pinto, H., Maskrey, V., Swift, L., Rumball, D., Wagle, A., Holland, R. (2010). “The SUMMIT trial: A field comparison of buprenorphine versus methadone maintenance treatment.” Journal of Substance Abuse Treatment 39: 340-352.
SAMHSA (2007). Results from the 2006 National Survey on Drug Use and Health: National Findings. Substance Abuse and Mental Health Services Administration. Rockville, MD, Office of Applied Studies.
Schuman-Olivier, Z., Albanese, M., Nelson, S. E., Roland, L., Puopolo, F., Klinker, L., & Shaffer, H. J. (2010). Self-treatment: Illicit buprenorphine use by opioid dependent treatment seekers. Journal of Substance Abuse Treatment, 39, 41-50.
Walley A.Y., A. J. K., Cheng D.M. (2008). “Office-based management of opioid dependence
with buprenorphine: clinical practices and barriers.” Journal of General Internal Medicine 23(9): 1393-1398.