The WAGER Vol. 5(45) – GP Intervention: Now or Never?
What role do general practitioners play in the prevention, diagnosis, and treatment of problem gambling? The answer is not clear. A study conducted by Sean Sullivan et al. (2000) attempted to determine whether intervention for problem gamblers was considered a legitimate role for GPs in New Zealand. In addition, the investigators attempted to clarify the extent of GPs knowledge of gambling related resources and their confidence in intervening when and if a patient is identified as a problem gambler.
Distributing questionnaires to GPs throughout New Zealand (n=100), Sullivan et al. split GP responses into four categories: one, general attitude toward prevention/intervention; two, beliefs as to the GPs role in a gambling disorder; three, knowledge; and four, perception of GP skills to intervene. With regard to general attitude, Sullivan and his associates discovered that GPs held favorable attitudes with respect to counseling patients (84%), influencing positive patient lifestyle (85%), and referring patients to non-medical professionals (91%). GPs surveyed also felt strongly about their role in supporting a problem gambler’s family (65%), with 72% disagreeing with the idea that doctors have little part to play in the treatment of problem gambling (Sullivan et al., 2000). With regard to GP knowledge of problem gambling, 89% of those surveyed reported that they view problem gambling as an addiction, while approximately half (51%) considered gambling as significant a problem as drug and alcohol abuse.
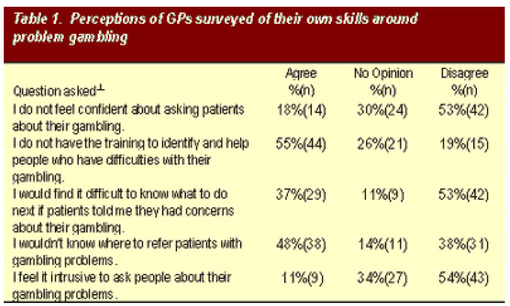
Variation among GP respondents was greatest in the fourth category of questionnaire responses: GPs perceptions of skills to intervene once a gambling problem is recognized. Indeed, while 54% of the GP respondents indicated that they would not lack confidence in asking patients about gambling problems, 19% felt their training was sufficient to allow them to successfully intervene. In addition, over one-third (37%) of the respondents admitted they would have some difficulty knowing what to do if a patient reported concerns about gambling, with almost half (48%) not knowing where to refer patients with gambling problems. Table 1 below summarizes these and other response patterns regarding GPs perception of their skills to handle gambling problems.
*Percentages rounded and might not add to 100%.
Sullivan et al. (2000) provide conclusions that are insightful but exploratory. While the data suggest GPs might have a problem concerning their competency and knowledge of resources to treat problem gamblers, such deductions are not conclusive. Indeed, the selected sample fails to include any differences with regard to the patient population the selected GPs treat. Some GPs might treat a population more prone to gambling problems, while others may see very little of these patients. This discrepancy can bias the Sullivan et al. results. Moreover, it is inaccurate to claim that survey respondents agree with a particular statement simply because they indicated that they disagree on the survey. For example, Sullivan and his associates conclude that 19% of GP respondents expressed confidence in their training to successfully intervene in a problem gambling situation. However, this 19% actually was disagreeing with the statement that they did not have the training to successfully intervene. As such, it remains unclear if this group actually believes that they have the full ability to successfully intervene. In addition, further research needs to address the significant amount of "no opinion" responses. Sullivan et al. (2000) assert that such responses were due to ambivalence, undetermined attitudes, or lack of knowledge. Until these "no opinion" responses are scrutinized closely, final interpretations of their findings must remain uncertain.
The work of Sullivan et al. remains valuable. It addresses an aspect of the gambling treatment system that could become more problematic since GPs represent a group of clinicians on the front line who are likely to encounter problem gamblers before other human service providers. As has been observed with alcohol and other drug treatments (Vander Bilt, Hall, Shaffer, & Higgins-Biddle, 1997), barriers to intervention include the perception of skills to address problem gambling as well as availability of resources (or lack thereof). As Sullivan et al. (2000) assert, more attention must focus upon the diagnostic ability of GPs to recognize problem gambling for sub sequential aspects of gambling treatment to be effectively developed.
[1] Thirteen of the twenty-seven questions were modeled on those of an alcohol study involving GPs (Roche et al., 1991), while ten additional questions were extracted from a similar study on nurses (Adams, 1994). Four questions involved additional aspects on gambling including GP role and knowledge.
References
Adams, P. (1994). Research consultant involvement in hospital intervention projects: nurse responses to intervention procedures. Auck: Bridgeway Family Psychiatric Center.
Roche, A., & Richard, G. (1991). Doctors’ willingness to intervene in patients’ drug and alcohol problems. Social Science and Medicine, 33, 1053-1061.
Sullivan, S., Arroll, B., Coster, G., Abbott, M., & Adams, P. (2000). Problem gamblers: do GP’s want to intervene? New Zealand Medical Journal, 113(1111), 204-207.
Vander Bilt, J., Hall, M. N., Shaffer, H. J., & Higgins-Biddle, J. C. (1997). Assessing substance abuse treatment provider training needs: screening skills. Journal of Substance Abuse Treatment, 14(2), 163-171.